-
Book Appointments & Health Checkup Packages
- Access Lab Reports
-
-
Book Appointments & Health Checkup Packages
-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Anesthesiology
- Cardiology
- Cardiothoracic Vascular Surgery
- Dialysis
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Medical Gastro
- Minimal Access Surgery
- Neonatology & NICU
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Spine Care
- Sports Medicine
- Urology
Other Specialities
- Andrology
- Bariatric Surgery
- Bone Marrow Transplantation
- Cancer Care/Oncology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Fetal Medicine
- General Surgery
- Genetics
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Healthy Weight Clinic
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Medical Oncology
- Nuclear Medicine
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric And Child Care
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Bhubaneswar
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Emergency Health Card
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Childhood Incontinence Clinic
Childhood Incontinence Clinic in Bhubaneswar
At Manipal Hospitals in Bhubaneswar, Odisha, our Paediatric Urology department offers specialised care for childhood incontinence, a common condition affecting children that involves the involuntary loss of bladder control. Childhood incontinence can manifest as bedwetting (nocturnal enuresis), daytime accidents, or a combination of both. This condition can have a significant impact on a child’s emotional well-being and self-esteem, making early diagnosis and treatment crucial.
Childhood incontinence clinic in Bhubaneswar provides treatment thorough evaluation to determine the underlying cause, which could range from delayed bladder development to urinary tract infections or more complex urological conditions. Our paediatric urologists work closely with each child and their family to develop a personalised treatment plan that may include behavioural therapies, medications, or, in some cases, surgical interventions.
FAQ's
The involuntary flow of urine during sleep is referred to as bedwetting, or nocturnal enuresis, whereas the involuntary urination that occurs during the day, or diurnal enuresis, is known as daytime wetting.
A child with encopresis, also known as faecal incontinence, lacks control over their bowel movements, which results in the unintentional passage of faeces.
Distinct underlying causes and treatment modalities may be associated with distinct types of childhood incontinence, underscoring the significance of accurate diagnosis and management based on the specific needs of each child.
Several forms of incontinence in childhood exist. These are:
- Bedwetting, or nocturnal enuresis, occurs during sleep and is common in children over the age of five.
-
Diurnal enuresis happens during the day and is often caused by infections or an overactive bladder.
-
Encopresis refers to the passage of stool due to chronic constipation.
-
Urge incontinence, characterised by sudden urges to urinate, is associated with neurological disorders or an overactive bladder.
-
Functional incontinence, which involves difficulties reaching the bathroom in time, is caused by physical or mental challenges.
Accurate identification of the type of incontinence helps tailor care to meet the specific needs of each child.
Childhood incontinence may indicate underlying medical issues such as urinary tract infections, constipation, neurological issues, or psychological strain that need to be properly diagnosed and treated. Early identification and treatment of underlying issues is essential for the successful management of incontinence in children as well as for the development of their self-esteem and general well-being. A medical professional's evaluation may be required if incontinence continues after the typical age of five years old, at which point a child can usually regulate their bladder.
The following are the average age milestones for children to reach bladder and bowel control:
-
18–24 Months: Many kids start to exhibit indicators that they're ready for potty training, like wanting to use the restroom, expressing pain in their dirty nappies, and being dry for extended periods of time.
-
2-3 years: During this time, daytime bladder control is frequently attained. Most kids can start using the restroom regularly during the day and remain dry for several hours.
-
3–4 Years: In most cases, children have gained bowel control and use the toilet regularly.
-
4–5 Years: Urinary control at night is usually accomplished. Most kids remain dry through the night by the time they are five years old, while others might still sometimes void their beds (nocturnal enuresis).
-
5–7 Years: Most kids at this age can control their bowel and bladder completely throughout the day and at night. If problems persist, more testing might be necessary to rule out underlying medical or psychological disorders.
Urinary incontinence symptoms can include more frequent trips to the bathroom due to increased urgency to urinate, in addition to urine leaking. Those who have incontinence in their urine may also be more vulnerable to difficult-to-treat urinary tract infections. Children who restrict their fluid intake due to fear of accidents run the risk of being dehydrated and making their constipation worse. It's critical to treat these symptoms as soon as possible in order to ensure appropriate management and enhance general health.
Children's nocturnal enuresis may result from a variety of factors, including overproduction of urine, insufficient bladder capacity, genetic susceptibility, sleep difficulties, mental stress, constipation, urinary tract infections, or anatomical abnormalities. For customised treatment, which may include behavioural techniques, medication, or the treatment of underlying medical conditions, determining the reason is essential.
To diagnose a child, medical professionals ask about bowel habits, underlying medical conditions, and a complete medical history. Through a comprehensive physical examination, the child's bowel and bladder functions can be assessed. Imaging procedures such as voiding cystourethrography or ultrasounds can be used to evaluate the anatomy and physiology of the urinary system. Urine or stool analysis can also be used to detect infections or other abnormalities. Treatment suggestions for childhood incontinence may be impacted by the findings of specialised testing, such as urodynamic examinations, which provide more details regarding the functioning of the bladder.
There are differences in the causes and treatments of nocturnal enuresis (bedwetting) and daytime enuresis (diurnal). The daytime is frequently associated with constipation, UTIs, hyperactive bladders, and uncommon anatomical problems. Genetics, delayed maturation, excessive urination at night, sleep difficulties, or stress can all contribute to nocturnality. Underlying causes are addressed, behavioural techniques like timed voiding or alarms are used, and drugs like desmopressin are used as treatments. For each kind, management targets particular triggers.
In behavioural therapies like bladder training, planned voiding and reinforcement approaches are employed to encourage bladder control. Through steady training, moisture alarms can assist children in responding to signals from their bladders, allowing them to wake up when they start to wet the bed. Dietary changes, such as abstaining from coffee and alcohol right before bed, may lessen nocturnal enuresis. Doctors may prescribe drugs or anticholinergics to decrease urine production or enhance bladder function. Urinary tract infections and constipation management are two underlying medical issues that need to be addressed to fully cure childhood incontinence.
Children who are constipated may experience difficulties with bladder control as a result of physical strain on the bladder, which can result in urgency and frequent urination. Moreover, it may impair bladder feeling and set off excessive bladder reflexes. Complicating matters are behavioural issues, such as retaining pee because of discomfort, and psychological effects, like humiliation. In order to enhance overall continence and restore regular bowel function, constipation is treated with dietary changes, medicines, and behavioural therapy.
Teaching kids to frequently empty their bladders and not to hold onto urine for long periods of time is an important part of promoting healthy bladder habits in kids. Developing regular bathroom routines, such as setting aside time for specific potty breaks, can improve bladder control. A diet rich in fibre and sufficient fluid consumption helps ease constipation by decreasing the pressure in the bladder and minimising the chance of difficulties. By lowering stress through counselling or relaxation techniques, children's risk of incontinence can be reduced, and their overall bladder health can be improved.
Teaching kids to frequently empty their bladders and not to hold onto urine for long periods of time is an important part of promoting healthy bladder habits in kids. Developing regular bathroom routines, such as setting aside time for specific potty breaks, can improve bladder control. A diet rich in fibre and sufficient fluid consumption helps ease constipation by decreasing the pressure in the bladder and minimising the chance of difficulties. By lowering stress through counselling or relaxation techniques, children's risk of incontinence can be reduced, and their overall bladder health can be improved.
Children can learn to control their bladder function using behavioural strategies such as visual signals, bedwetting alarms, relaxation exercises, hydration management, scheduled voiding, and positive reinforcement. By creating routines, controlling urgency, and encouraging dry times, these techniques boost self-esteem and lessen the effects of incontinence on day-to-day living. Effective management of infantile incontinence is ensured by customised implementation and continued assistance.
By comforting the child, avoiding placing guilt or blame on them, and acknowledging their accomplishments in managing incontinence, parents can create a helpful environment. Promoting transparent communication enables kids to voice their preferences and worries, enabling them to participate actively in treatment choices. Working together with medical specialists assures that children will have access to continuing assistance and specialised care that is suited to their requirements, which promotes the best possible outcomes for controlling childhood incontinence.
Psychological factors like stress, anxiety, low self-esteem, parental pressure, fear of punishment, trauma, and body image issues can all have an impact on childhood incontinence. For management to be effective, these aspects must be addressed in addition to behavioural and medicinal approaches. The provision of emotional support, promotion of open communication, and cultivation of a pleasant atmosphere can substantially aid youngsters in managing and surmounting the obstacles linked to incontinence.
While a lot of children grow out of incontinence on their own as they get older, some might need help from medical professionals, behavioural therapists, or medications to control it. Treatment outcomes are dependent on several variables, including the severity of the ailment, the child's reaction to therapy, and treatment compliance. For the best results in treating child incontinence, the treatment strategy may need to be modified and monitored regularly.
A comprehensive process that includes a patient's medical history, physical examination, analysis of their voiding diaries, urinalysis, imaging studies, specialised testing (such as cystoscopy or urodynamic studies), and psychological evaluation is used to diagnose incontinence in children. These procedures aid in the identification of potential reasons, including infections, anatomical anomalies, or psychological variables affecting bladder control. Customised treatment programmes that enhance the child's well-being and successfully control symptoms are made possible by early diagnosis.
Children with encopresis (stool incontinence) are usually treated with laxatives or stool softeners for maintenance therapy after a bowel cleanout to eliminate impacted stool. Important interventions include dietary adjustments, potty training, behavioural treatment, education, and treating underlying causes like stress or illnesses. Monitoring and follow-up on a regular basis guarantee the efficacy of the treatment and promote improvements in overall health and bowel control.
Home Bhubaneswar Specialities Paediatric-and-child-care Childhood-incontinence-clinic

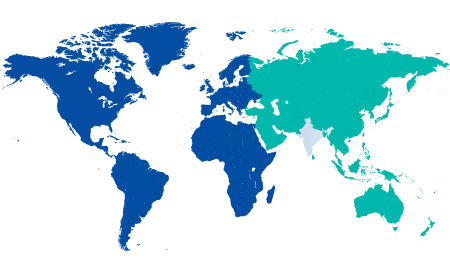
You’re on Our Indian Website
Visit the Global site for International patient services










