-
Book Appointments & Health Checkup Packages
- Access Lab Reports
-
-
Book Appointments & Health Checkup Packages
-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Anesthesiology
- Cardiology
- Cardiothoracic Vascular Surgery
- Dialysis
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Medical Gastro
- Minimal Access Surgery
- Neonatology & NICU
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Spine Care
- Sports Medicine
- Urology
Other Specialities
- Andrology
- Bariatric Surgery
- Bone Marrow Transplantation
- Cancer Care/Oncology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Fetal Medicine
- General Surgery
- Genetics
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Healthy Weight Clinic
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- IVF and Infertility
- Medical Oncology
- Nuclear Medicine
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric And Child Care
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Bhubaneswar
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Emergency Health Card
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Neuro Intensive Care
Neuro Intensive Care in Bhubaneswar
The Paediatric Intensive Care Unit (PICU) offers neuro-intensive care for critically ill paediatric patients. It helps in diagnosing and treating ailments affecting the neurological system, such as the brain, spinal cord, nerves, and muscles. Our state-of-the-art technology, coupled with a highly skilled team of paediatric medical professionals, is equipped to address several neurological conditions, such as traumatic brain injury, intracranial haemorrhage, brain tumours, meningitis, encephalitis, seizures, stroke, and other neurological disorders.
As a leading facility in the state of Odisha, we are committed to incorporating methods to stabilise critically ill paediatric patients in order to prevent secondary neurological damage, enhance neurological function, and provide comprehensive support to parents, addressing their concerns and doubts.
Consult our PICU hospital if you need Neuro-intensive Care in Bhubaneswar.
FAQ's
Several conditions necessitate neuro-intensive care for paediatric patients. These include acute disseminated encephalomyelitis (ADEM), autoimmune encephalitis, brain vessel malformations with new and severe complications, cardiac arrest, brain and spinal cord malignancies, hepatic encephalopathy, infections of the brain and spinal cord, intracranial haemorrhage, mitochondrial disorders, neurological side effects of chemotherapy, radiation, and other medications, neuromuscular disorders such as Guillain-Barre Syndrome (GBS), infant botulism, and myasthenia gravis, seizures, status epilepticus, stroke, and traumatic brain and spinal cord injuries.
Types of diagnostic procedures and treatment interventions depend on the type of condition and the individual needs of a child. Common diagnostic procedures and treatment interventions include:
-
Electroencephalogram (EEG): A procedure involving the evaluation of brain activity in paediatric patients using electrodes placed on the scalp. Primarily aids in diagnosing and treating seizures.
-
Imaging Tests: Imaging tests such as magnetic resonance imaging (MRI) and computer tomography (CT scan) help in identifying physiological and anatomical issues in the brain and skull, such as inflammation, tumours, fractures, and other related brain-related issues.
-
Electromyography (EMG): A test that helps in assessing the electrical activity of the muscle in response to nerve stimulation. The test is primarily used to identify any neuromuscular abnormalities.
-
Nerve Conduction Studies (NCS): It is also called the nerve conduction velocity (NCV) test, and it is employed to measure electric impulses through the child’s nerves, identifying any nerve damage.
-
Lumbar Puncture: This involves obtaining a sample of cerebrospinal fluid (CSF) from the lower back with the help of a sterile needle and is used to diagnose neurological infections, inflammation, and other ailments.
-
Genetic Testing and Biopsies: Help identify genetic abnormalities and diagnose brain tumours or infections.
-
Other treatment options may include but are not limited to, Botulinum Injections, Vagus Nerve Stimulation (VNS), and Deep Brain Stimulation (DBS).
The duration of your child’s hospital stay depends on the severity of their condition and their response to treatment. Some children may have a short-term stay in the PICU, while critically ill paediatric patients diagnosed with complex neurological conditions may require extended care.
Paediatric patients in the PICU are closely monitored by a team of paediatric medical professionals, and your child will be assessed frequently for their condition. You can also expect consultations or communications from your child's specialist, who supports you in the decision-making process. Your medical provider also addresses any concerns you may have.
Neuromonitoring is a central component of modern neuro-intensive care, which aims to prevent secondary neurological insults from hypotension, hypothermia, hypoxia, hypoglycemia, intracranial hypertension, and seizures. These insults have the potential to cause severe brain injuries, leading to unfavourable outcomes.
There are various treatment approaches for children, depending on the severity of the seizures. Healthcare providers typically begin with anti-epileptic drugs. If these medications cause side effects, surgical interventions such as VNS or DBS may be considered. Your child’s healthcare provider will educate you on the procedures, potential complications, and risks and assist you in making well-informed decisions regarding your child’s health.
The long-term effects and prognosis for children receiving neuro-intensive care depend on factors such as the type and severity of the diagnosed neurological condition or injury, as well as their general health and ability to recover. Some children may experience full recovery, while others may face prolonged neurological disorders or disabilities. Your medical provider will inform you of your child’s prognosis and the necessary course of action you can take.
After recovery, your child may transition to less intense monitoring and care or be completely discharged from the hospital. The decision to transition depends on your child’s readiness and health stability. In some cases, children may still have a long road to recovery. You must collaborate frequently with your child's specialist and address your concerns. This ensures that your child receives proper guidance and support for future treatment and care.
Home Bhubaneswar Specialities Paediatric-intensive-care-unit Neuro-intensive-care-treatment

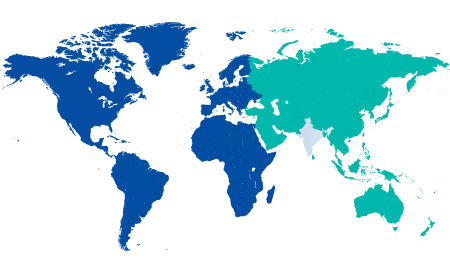
You’re on Our Indian Website
Visit the Global site for International patient services










