
Listen to article
Loading audio...
Gastrointestinal bleeding refers to bleeding that occurs in any part of the gastrointestinal tract, which includes the oesophagus, stomach, small intestine, large intestine, rectum, and anus. It can range in severity from mild to life-threatening. The causes of gastrointestinal bleeding can vary and may include ulcers, gastritis, diverticulosis, colon polyps, Crohn's disease, and tumours. Gastrointestinal bleeding occurs when there is a rupture or erosion in the blood vessels that line the digestive tract. As blood vessels break, blood can be released into the digestive system, leading to visible or hidden bleeding.
Types of Gastrointestinal Bleeding
Gastrointestinal bleeding can originate from various segments of the digestive tract, giving rise to different types of bleeding episodes. The two main categories are upper gastrointestinal bleeding (UGIB) and lower gastrointestinal bleeding (LGIB).
-
Upper Gastrointestinal Bleeding (UGIB): Upper gastrointestinal bleeding refers to bleeding that occurs in the upper part of the digestive system, primarily the oesophagus, stomach, and the initial portion of the small intestine (duodenum). UGIB often results in the presence of blood in the vomit (hematemesis) or dark, tarry stools (melena).
-
Lower Gastrointestinal Bleeding (LGIB): Lower gastrointestinal bleeding originates from the lower portion of the digestive tract, including the colon, rectum, and anus. Bleeding in this region often results in bright red or maroon-coloured stools (hematochezia).
Dr. Rohit Sureka, Consultant - Gastroenterology, Manipal Hospitals Jaipur, explains the problem of blood in stool in this insightful video. Watch the complete video to learn the causes and treatments for the problem.
Common Causes of Gastrointestinal Bleeding
Gastrointestinal bleeding can stem from a variety of underlying conditions and factors. Understanding the common causes behind these bleeding episodes is vital for both identifying potential risks and seeking appropriate medical attention.
-
Peptic Ulcers: Peptic ulcers are open sores that develop on the inner lining of the stomach, the upper part of the small intestine (duodenum), or the oesophagus.
-
Gastritis: Gastritis refers to inflammation of the stomach lining. Chronic gastritis can cause the lining to wear away, leading to erosions and bleeding.
-
Colorectal Polyps and Cancer: Abnormal growths called polyps can form in the colon or rectum. While most polyps are benign, some can become cancerous over time.
-
Esophageal Varices: Esophageal varices are enlarged veins in the oesophagus that commonly develop as a complication of liver disease, particularly cirrhosis. These veins can rupture and cause significant, life-threatening bleeding.
-
Mallory-Weiss Tears: Mallory-Weiss tears are small tears or lacerations in the lining of the oesophagus or stomach. They often result from forceful vomiting, coughing, or retching and can lead to bleeding.
-
Diverticulosis and Diverticulitis: Diverticulosis involves the formation of small pouches (diverticula) in the colon wall. These pouches can become inflamed or bleed, leading to diverticulitis and gastrointestinal bleeding.
-
Gastroesophageal Reflux Disease (GERD): GERD is a chronic condition where stomach acid flows back into the oesophagus, irritating. Severe cases of GERD can lead to inflammation, erosions, and bleeding in the oesophagus.
-
Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease and ulcerative colitis are types of IBD that involve chronic inflammation and ulceration in the digestive tract. These conditions can lead to bleeding and other complications.
Symptoms and Prevention Techniques of Gastrointestinal Bleeding
Gastrointestinal bleeding can manifest through various symptoms and requires prompt medical attention to prevent complications. In this section, we'll delve into the common symptoms associated with gastrointestinal bleeding and ways to prevent this condition effectively. Consult the best gastroenterologists in Bangalore in case you notice any of the below symptoms.
Symptoms of Gastrointestinal Bleeding
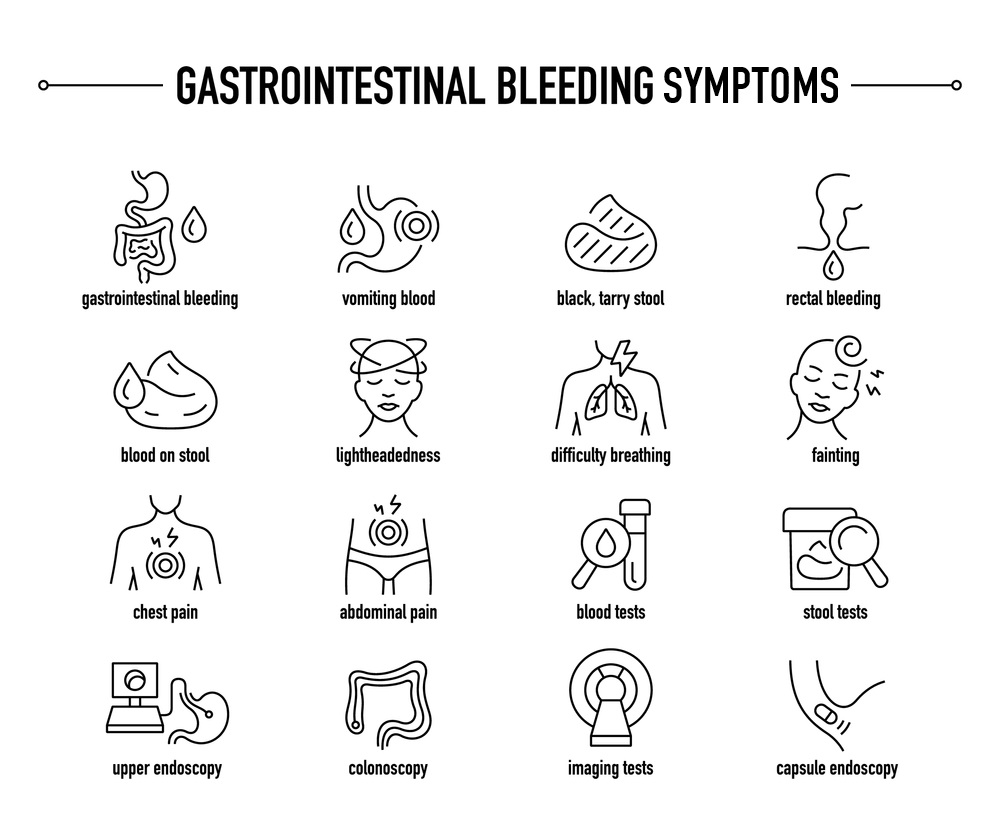
The symptoms of gastrointestinal bleeding can vary depending on the location and severity of the bleeding. Some of the key symptoms to watch for include:
-
Hematemesis (Vomiting Blood)
-
Melena (Dark, Tarry Stools)
-
Hematochezia (Bright Red Stools)
-
Anaemia and Fatigue
Prevention Techniques
Preventing gastrointestinal bleeding involves a combination of lifestyle adjustments, addressing underlying conditions, and adopting protective measures. Let’s see how you can minimise the risk of experiencing GI bleeding.
-
Healthy Dietary Choices
-
Responsible Medication Use
-
Manage Underlying Conditions
-
Avoid Alcohol and Tobacco
-
Regular Check-ups and Screenings
-
Stress Management
-
Hygiene and Food Safety
-
Medication Adherence
-
Stay Informed.
Treatment Options for Gastrointestinal Bleeding
Treatment of gastrointestinal (GI) bleeding depends on the cause and location of your bleeding. Here are some treatment options:
1. Diagnostic Procedure: In procedures such as upper GI endoscopy, lower GI endoscopy, colonoscopy, flexible sigmoidoscopy, or laparotomy, medical professionals can halt gastrointestinal bleeding. This can be achieved by employing instruments through an endoscope, colonoscope, or sigmoidoscope to:
-
Administer medications directly to the bleeding area.
-
Apply therapeutic measures to the site of bleeding and the adjacent tissue using techniques like heat probes, electric currents, or lasers.
-
Secure affected blood vessels using bands or clips, effectively closing them off.
2. Medicines: When infections or ulcers lead to bleeding within your gastrointestinal tract, you can be given medications to address the issue.
3. Surgical Procedures: In cases where bleeding is severe, surgical options may be considered. This could involve removing a bleeding ulcer or repairing damaged blood vessels through laparoscopy or a laparotomy.
Complications and Consequences of Gastrointestinal Bleeding
Gastrointestinal bleeding, when not promptly managed, can lead to serious complications. Severe bleeding can result in hemorrhagic shock, causing a drop in blood pressure and depriving organs of oxygen. Recurrent bleeding can worsen anaemia, leading to fatigue and weakness. Hospitalisation may be necessary for monitoring and interventions to stop bleeding. Surgical procedures might also be required if conservative treatments fail. The psychological impact, increased mortality risk, and overall health deterioration highlight the importance of seeking timely medical attention and effective management strategies. Visit the best gastroenterology hospital in Bangalore to get the best treatment available.





















 6 Min Read
6 Min Read












