Drug resistant and multidrug resistant bacteria have emerged as major concerns both inside and outside the hospital environment. This problem is especially of concern in the intensive care unit wherein the risk of selection and emergence of resistant pathogens is high due to the pressure and need for using broad-spectrum anti-microbial regimen. Resistance is a measure of the decreased ability of an anti-microbial agent to kill or inhibit the growth of a microbial organism. For quantitative systems the measure of a drug activity is Minimum Inhibitory Concentration (MIC). Break points that define the thresholds of susceptibility for each bacteria-drug combination is defined by different groups. The drug is considered susceptible if the MIC is below the breakpoint.
Multidrug Resistant (MDR) Bacteria
Multidrug resistant bacteria are organisms which have acquired resistance to multiple unrelated classes of antibiotics. MDR organisms of greatest concern include Methicillin-resistant Staphylococcus aureus (MRSA), Vancomycin-resistant Enterococcus (VRE), Drug-resistant Streptococcus pneumonia (DRSP) and MDR gram negative bacilli (MDR GNB) like Pseudomonas, Acinetobacter, Klebsiella, Enterobacter and other species.
MRSA:
By 2005, about 65% of healthcare associated infections were caused by MRSA. MRSA resistance is mediated by the Mec A gene, which encodes for the Penicillin-binding protein (PBP) with decreased affinity to nearly all beta-lactam antibiotics. The drug of choice for treatment of MRSA is the Glycopeptide Vancomycin. Newer antibiotics effective against MRSA include Oxazalidinone like Linezolid, newer glycopeptides (like Daptomycin), Tetracycline (like Tigecycline) and Telavancin. However, at present the incidence of Vancomycin-resistant Staphylococcus aureus (VRSA) is extremely low and not reported in India.
Multidrug-resistant Enterococci and Vancomycin-resistant Enterococci
Enterococci are normal commensals in the human gastrointestinal tract. E faecalis and E faecium are of clinical importance. Faecalis species is commoner for community-acquired infections, while the latter commonly causes nosocomial infections. E faecalis is often sensitive to Ampicillin, Carbapenems etc. E faecium are more virulent and requires treatment with Vancomycin. Common sources of infections include UTI, device-related blood stream infections and others. There is increasing incidence of Vancomycin resistance described in E faecium requiring treatment with newer agents like Daptomycin, Tigecycline and Telavancin. But it is important to note that Tigecycline is a bacteriostatic drug and only useful for the management of soft tissue and intra-abdominal infections.
Drug-resistant Streptococcus pneumonia
This is an extremely rare problem at present. Despite the increasing incidence of penicillin resistance, the overall prevalence of resistance for penicillin and Cephalosporins still remains low.
Antibiotic-resistance in gram-negative bacteria
Infections with resistant gram-negative bacteria are a significant problem causing high mortality and morbidity in critically ill patients. Commonest mechanism of resistance includes production of Beta lactamases which hydrolyses the beta-lactam antibiotics and production of Carbapenemases.
Increasing resistance has been noted to Flouroquinolones and Aminoglycosides as well. In view of the increasing resistance to conventional antibiotics, Tigecycline and Colistin was used as treatment strategies but now, resistance has developed to these as well. ESBL-producing Enterobacteriaceae can be treated with Piperacillin-tazobactam or Carbapenems like Meropenem. Carbapenemase producing Enterobacteriaceae is also an increasing concern. For management of these bacteria, Colistin and Tigecycline seem to be the only option. However, Tigecycline cannot be used for bacteremia and urosepsis, as Tigecycline is a bacteriostatic drug.
Management of non-fermenting GNB (like Pseudomonas, Acinetobacter species and S Maltophilia) is also becoming increasingly challenging. Colistin and Tigecycline seems to be the only available treatment modality. S Maltophilia is sensitive to only Levofloxacin and Co-trimoxazole. S Maltophilia is innately resistant to even Colistin. Some emerging data suggests that pseudomonas may be sensitive to Doripenem, inspite of resistance to other Carbapenems. But the same needs more studies to establish this fact.
Resistance to anaerobic agents in the ICU
Recent data have shown an increasing resistance to Clindamycin and Moxifloxacin, particularly to Bacteroides fragilis. However, the incidence of resistance to Metronidazole remains extremely low (< 1%).
Management of antimicrobial resistance
A multi-intervention strategy is essential to control the spread of antimicrobial resistance. This varies from legislation to local practices to infection control practices at the individual bedside. The CDC (Centers for Disease Control and Prevention) has strategised a series of steps to prevent antimicrobial resistance in healthcare settings.
Regulation of antimicrobial usage in the ICU
This is a very complex issue requiring the balancing between the prompt start of broad-spectrum cover in critically ill patients to rapid appropriate de-escalation in preventing resistance. This requires a robust antimicrobial stewardship programme. This has to be guided by adequate knowledge of the local resistance patterns of respective healthcare facility.
Infection prevention
It is important to take steps to prevent transmission of infection between patients. Infection control practices may be “bundled” together into global measures to prevent infections and decrease the risk of antibiotic resistance.
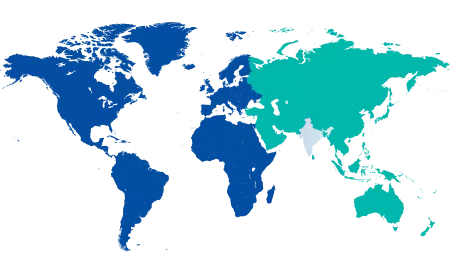
Thus in summary, infections with multi-drug resistant bacteria are a growing problem across the world. Resistance patterns are changing and most gram negative bacteria currently are MDR at least in the setting of nosocomial infections. Currently, there are no available antibiotics in the pipeline for treatment of gram negative infections. Prevention of infections and judicious use of antibiotics seem to be the solution to reduce the burden of drug resistant infections.
Dr. Sunil Karanth MD, FNB, EDIC, FCICM (Aus/NZ)
Chairman, Critical Care Medicine,
Manipal Health Enterprises Private Limited.
Disclaimer: The views expressed in this article are of the writer and not of the hospital.






















 2 Min Read
2 Min Read