Brain-eating amoeba, also known as Naegleria fowleri, is a microscopic organism that poses a rare but deadly threat to human health. Found in warm freshwater environments such as lakes and poorly maintained swimming pools, these amoebas typically lead harmless lives. However, when they enter the human body through the nose, they can cause a severe and often fatal infection known as primary amebic meningoencephalitis (PAM).
Understanding the nature of brain-eating amoebas and the primary species responsible for infection is crucial to comprehend the severity of this condition. In the subsequent sections of this blog, we will delve deeper into the symptoms, diagnosis, treatment options, and preventive measures associated with brain-eating amoebas. Keep reading till the end to know more about these elusive organisms, and get the knowledge necessary to protect yourself and your loved ones.
Symptoms and Diagnosis of Brain-eating Amoeba
When it comes to brain-eating amoeba infection, early detection is key to saving lives. Understanding the symptoms and the diagnostic process can empower individuals to seek timely medical intervention. In this section, we will explore the common symptoms experienced by those infected with brain-eating amoeba, discuss how healthcare professionals diagnose the infection and emphasise the vital importance of early detection and prompt medical intervention.
Common Symptoms of Brain-Eating Amoeba Infection
Brain-eating amoeba infection progresses rapidly and can lead to severe neurological complications. While the incubation period varies, symptoms typically manifest within a few days of exposure. Some common symptoms experienced by individuals infected with brain-eating amoeba include:
1. Initial Symptoms
Initially, individuals may experience symptoms similar to those of a viral illness, such as headache, fever, nausea, vomiting, and a stiff neck. Also, read the blog on Different types of headaches to analyze the symptoms better.
2. Neurological symptoms
As the infection progresses, it can cause severe neurological symptoms, including a sudden onset of severe headache, seizures, altered mental status, confusion, hallucinations, difficulty with coordination, and coma. It is advisable to consult the top neurologists in Bangalore for a detailed diagnosis and treatment plan if you suspect any symptoms as such.
Diagnosis of Brain-Eating Amoeba Infection
Diagnosing brain-eating amoeba infection requires a combination of clinical evaluation, laboratory tests, and neuroimaging studies. Healthcare professionals employ the following diagnostic methods:
-
Medical History and Physical Examination: Physicians will assess the individual's symptoms, medical history, and recent activities involving freshwater exposure, and perform a thorough physical examination.
-
Cerebrospinal Fluid (CSF) Analysis: A lumbar puncture (spinal tap) is performed to collect a sample of cerebrospinal fluid. Laboratory analysis of the CSF can help identify specific markers of brain inflammation and the presence of the amoeba.
-
Microscopic Examination: Microscopic examination of the CSF or tissue samples may reveal the presence of the amoeba trophozoites.
-
Polymerase Chain Reaction (PCR) Testing: PCR testing can be used to detect the genetic material of the amoeba in CSF or tissue samples, offering a highly sensitive and specific diagnostic method.
Causes and Risk Factors of Brain-Eating Amoeba Infection
Understanding the causes and risk factors associated with brain-eating amoeba infection is essential for preventing its occurrence. In this section, we will delve into the environmental sources where brain-eating amoeba can be found, explore the routes of transmission leading to infection, and identify specific risk factors that increase the likelihood of encountering this deadly amoeba.

Environmental Sources of Brain-Eating Amoeba
Brain-eating amoeba, particularly Naegleria fowleri, can be found in various warm freshwater environments. These include:
-
Lakes, Ponds, and Rivers: Warm freshwater bodies, especially those with low water levels and stagnant conditions, can harbour the amoeba.
-
Hot Springs and Geothermal Areas: Geothermal environments, such as natural hot springs or thermal waters, provide ideal conditions for the growth and proliferation of brain-eating amoeba.
-
Poorly Maintained Swimming Pools: Swimming pools that are inadequately chlorinated, improperly cleaned, or left untreated can become breeding grounds for the amoeba.
It is important to note that brain-eating amoeba does not thrive in saltwater environments, such as oceans and seas.
Infection Occurrence and Routes of Transmission
Brain-eating amoeba infection occurs when water containing the amoeba enters the body through the nose. The primary routes of transmission include:
-
Water-related Activities: Activities involving exposure to warm freshwater, such as swimming, diving, water sports, or engaging in nasal irrigation using contaminated water, can introduce the amoeba into the nasal passages.
-
Inhalation: In rare cases, inhalation of contaminated water droplets, such as through the use of improperly cleaned or contaminated water sources (e.g., neti pots, nasal wash bottles), may also lead to infection.
Once the amoeba enters the nasal passages, it can migrate along the olfactory nerves and reach the brain, leading to the development of primary amebic meningoencephalitis (PAM).
Risk Factors for Brain-Eating Amoeba Infection
Several factors can increase the likelihood of encountering and becoming infected with brain-eating amoeba:
-
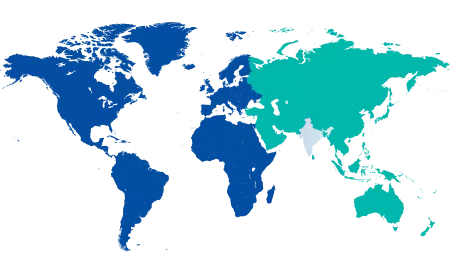
Hot climate: Brain-eating amoeba infections are more prevalent in regions with warm climates, particularly during hot summer months when water temperatures are higher.
-
Freshwater Exposure: Activities involving exposure to warm freshwater, such as swimming or diving in lakes, rivers, or hot springs, increase the risk of encountering brain-eating amoeba.
-
Nasal Passages Vulnerability: Certain activities or conditions that promote the entry of water into the nasal passages, such as diving or jumping into the water, using contaminated water for nasal irrigation, or having nasal sinus conditions, may heighten the risk of infection.
-
Young Age: Children and young adults are more susceptible to brain-eating amoeba infection, possibly due to higher rates of water-related activities and potentially more vulnerable nasal passages.
-
Immunocompromised Individuals: People with weakened immune systems, such as those with certain medical conditions or undergoing immunosuppressive therapy, may be at higher risk of developing severe brain-eating amoeba infections.
If anyhow your amoeba symptoms get triggered, visit the top neurology hospital in Bangalore immediately.
Treatment and Management of Brain-Eating Amoeba Infection
Treating brain-eating amoeba infection requires a comprehensive approach to combat the rapid progression of the disease. The following treatment options may be utilised:
-
Antifungal and Antimicrobial Medications: Medications, such as amphotericin B and azoles, are often used to target the brain-eating amoeba and control its growth. These medications are administered intravenously to reach the brain and combat the infection.
-
Adjunctive Therapies: Certain medications, such as antiepileptic drugs, may be prescribed to manage seizures, which can occur as a result of brain inflammation.
-
Hyperosmolar Therapy: In cases of severe brain swelling, hyperosmolar therapy may be employed to reduce intracranial pressure and alleviate symptoms.
Challenges and Limitations in Treating Brain-Eating Amoeba Infection
Treating brain-eating amoeba infection poses significant challenges due to several factors:
Delayed Diagnosis
The rapid progression of the infection and the rarity of the condition often lead to delayed diagnosis, making timely treatment challenging.
Limited Effectiveness of Available Medications
While medications like amphotericin B and azoles are used to treat brain-eating amoeba infection, their effectiveness is limited, and outcomes remain uncertain. The blood-brain barrier and the ability of the amoeba to form protective cysts pose challenges to successful drug delivery.
High Mortality Rate
Despite aggressive treatment, brain-eating amoeba infection has a high mortality rate. This underscores the need for early detection and intervention.
Scarce Research and Limited Clinical Trials
Due to the rarity of brain-eating amoeba infections, there is limited research and a lack of large-scale clinical trials to establish standardised treatment protocols.






















 5 Min Read
5 Min Read