-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Epilepsy Clinic
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Heart Care Clinic
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physical Medicine and Rehabilitation
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Broadway
- International Patients



Clinics








- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Diagnostic Tests
Diagnostic Tests for Male Infertility and Treatment in Broadway
At Manipal Hospitals, Broadway, Kolkata, our Department of Andrology provides comprehensive diagnostic testing to accurately identify and treat male reproductive and sexual health issues such as painful ejaculation, erectile dysfunction, etc. Our services include both routine and specialised testing, in addition to basic sperm analysis. We offer clinical sperm cryopreservation and advanced tests to assess male fertility through a thorough analysis.
While sperm count, motility, and morphology are crucial markers, other often-overlooked parameters can reveal conditions such as infections, prostatic diseases, or hormonal disorders. Early diagnosis is essential for tailored treatment and helps avoid unnecessary investigations for female partners.
For certain surgical procedures, two consecutive semen samples showing no sperm presence may be required, although exceptions exist for persistent non-motile sperm. Adherence to best practice guidelines ensures accurate reporting and informed decision-making for fertility management.
Consult our andrology hospital if you need Diagnostic Tests for Male Infertility and Treatment in Broadway.
FAQ's
Male infertility can have several causes. Physical causes include varicocele, testicles that have not descended, testicular injuries or surgeries, exposure to toxins or radiation, and excessive alcohol consumption are frequently to blame. Genetic disorders such as cystic fibrosis, Klinefelter's syndrome, and certain genetic variants may also be involved. Potential contributing factors include infections, STDs, and idiopathic infertility, the origin of which is yet unclear. Seeing a urologist and fertility expert can help identify the underlying causes of infertility problems.
A semen analysis tests several characteristics related to semen quality, such as sperm motility, concentration, morphology, and vitality. Other features of the semen are also measured that might aid in diagnosing particular illnesses. It is significant to highlight that the majority of measured criteria assist the doctor in determining the likelihood of particular infertility issues and particular treatment alternatives rather than offering a conclusive diagnosis of infertility.
Your fertility doctor will need a sperm sample before starting any reproductive therapy, such as Assisted Reproductive Technology (ART). The collection process is the same as for a semen analysis. Once collected, the sample is processed by removing the sperm from the surrounding seminal fluid. The sperm is then cleaned and inspected. After processing, the sperm can be used in treatments like intracytoplasmic sperm injection (ICSI) or in vitro fertilization (IVF) to aid in conception.
Your fertility specialist may organise a testicular biopsy to check whether there are issues with sperm production caused by a blockage. A testicular biopsy can also be used to diagnose testicular cancer or as a means of identifying the aetiology of other andrology-related problems, such as a mass in the testicles. Your physician using anaesthesia and/or a sedative to perform a testicular biopsy while you are conscious. The incision will be made, and a small sample of testicular tissue will be taken during the surgery. Your doctor might suggest skipping out on sexual activity for a week or two following this operation. If you have any other questions or concerns concerning this operation, please discuss them with your specialist.
The Sperm Chromatin Structure Assay is a test for male infertility. It accurately detects males who are less likely to achieve a full-term pregnancy spontaneously or with the use of assisted reproductive technology (ART). This is accomplished by ascertaining the proportion of sperm exhibiting elevated DNA fragmentation, denoted as the DNA Fragmentation Index (% DFI), in addition to the percentage of sperm possessing aberrant proteins (% HDS) and shape that could impede fertilisation. The exam is founded on tried-and-true methodologies and research.
Sperm in men is shielded from the body's immune system by the "blood-testis barrier," preventing the production of antibodies that could harm sperm. Breaching this barrier can lead to the production of anti-sperm antibodies, which may cause sperm agglutination or reduced motility when they attach to sperm. Testing semen, serum, or seminal fluid can determine the presence of antibodies. If there's decreased sperm motility, increased agglutination, or reduced sperm viability, an anti-sperm antibody assessment should be conducted. Females can also produce antibodies against sperm, warranting assessment if deemed necessary by a doctor.
Retrograde semen analysis is conducted for patients exhibiting decreased semen volume, altered seminal fluid pH, and/or azoospermia in their initial semen analysis. Retrograde ejaculation occurs when sperm is ejaculated into the bladder instead of out through the urethra. Men experiencing retrograde ejaculation may find sperm in their urine after sexual activity. This condition is often associated with medical conditions or surgical history, such as testicular cancer surgery, transurethral prostate surgery, or childhood bladder surgery. Additionally, individuals with medical disorders like diabetes, multiple sclerosis, or spinal cord damage may have an increased risk of retrograde ejaculation.
Home Broadway Specialities Andrology Diagnostic-tests

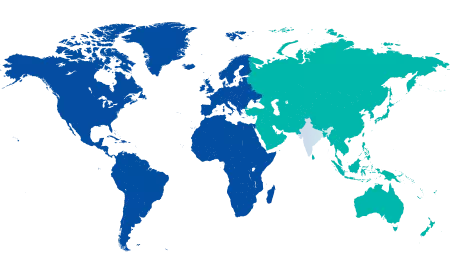
You’re on Our Indian Website
Visit the Global site for International patient services











