-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Epilepsy Clinic
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Heart Care Clinic
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physical Medicine and Rehabilitation
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Broadway
- International Patients



Clinics








- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Cardiac Resynchronization Therapy CRT and CRTD Implantation
Cardiac Resynchronization Therapy CRT and CRTD Implantation, Broadway
To decrease the mortality rate and extend the lifespan of individuals affected by various forms of heart failure, new therapies continue to emerge. Cardiac Resynchronization Therapy, also called CRT, is a ray of hope for heart failure patients. It is a clinically proven medical treatment that involves implanting a device to effectively improve the coordination of the heart's contractions by using electrical pulses that stimulate the heart muscles. This therapy is typically used for patients with heart failure and conduction abnormalities, such as left bundle branch block. At Manipal Hospitals in Broadway, our expert team of cardiologists and physicians providing Cardiac Resynchronization Therapy treatment services is trained in conducting CRT and CRT-D implantation procedures effectively in our internationally acclaimed cardiac catheterization lab.
CRT implantation is a specialised device, also called a biventricular pacemaker or CRT device, that is surgically implanted under the skin in the chest. It delivers synchronised electrical signals to both the left and right ventricles of the heart, helping them beat more efficiently. In cases where patients are at risk of life-threatening arrhythmias, a CRT device with a defibrillator function (CRT-D) may be implanted. CRT-D can deliver electrical shocks to restore normal heart rhythm if needed. Both CRT and CRT-D implantation significantly improve symptoms, quality of life, and treatment outcomes.
FAQ's
The doctor will recommend CRT treatment if you have:
- Moderate to severe heart failure, in which the pumping ability of the heart is compromised
- Weak or enlarged heart
- Medicines are unable to control heart failure
- Heart rhythm abnormality called left bundle branch block
- A heart condition that requires a pacemaker or defibrillator
- Experiencing symptoms of heart failure such as shortness of breath, exercise tolerance, and fatigue that impact your life
CRT devices are mainly of two types:
Cardiac Resynchronization Therapy with a Pacemaker (CRT-P): It is also called a biventricular pacemaker, a device used to treat certain stages of heart failure and irregular heart signalling. This sends signals to the lower heart chamber or ventricles to beat at the same time, thus ensuring that the heart is filled properly with blood.
Cardiac Resynchronization Therapy with a Defibrillator (CRT-D): This device combines a pacemaker with an implantable cardioverter-defibrillator (ICD). This is used in life-threatening conditions where people with heart failure are also at risk of sudden cardiac death. In the case of an irregular or dangerous heart rhythm, it can be detected and corrected by shocking the heart, resulting in a regular heartbeat.
- The doctor will order a series of tests (EKG, echocardiogram, cardiac MRI, and stress test) to assess your heart condition.
- Your medical history and current medication (including prescription, over-the-counter or supplements) will be studied.
- You may be asked to stop taking certain medications before the procedure to avoid any related complications.
- On the day of the procedure, an intravenous (IV) line will be inserted into your forearm or hand.
- A sedative medication will be administered through the IV to induce relaxation.
- Local anaesthesia will also be applied to numb the skin at the site where the CRT device will be implanted.
- During the procedure, you will be placed in the supine position and may be fully awake or lightly sedated, depending on specific circumstances and preferences.
- The surgery to implant the CRT device will typically take a few hours.
- The technique used during the procedure will vary depending on the type of CRT device being implanted.
- For implanting a pacemaker, a cardiologist will insert one or more wires, known as leads, into a major vein located under or near the collarbone.
- The doctor will navigate the wires to the heart using X-rays for proper placement.
- One end of each wire will be connected to the appropriate area in the heart, and the other end will be attached to the component of the CRT device responsible for delivering electrical pulses.
- When the desired effect is achieved, leads and catheters will be removed and incisions will be closed.
- To visualise and monitor the heart during the surgery, a transesophageal echocardiogram (TEE) is used.
- After the implantation of the CRT device, you will need to remain in the hospital overnight. Also, arrange for someone to drive you home after discharge.
- Most individuals can resume their normal activities within a few days after following the specific instructions provided by our care team.
- You will need to restrict upper body and arm movements and avoid strenuous exercise or heavy lifting for approximately a month post-procedure.
- Make sure to attend regular follow-up checkups with our cardiologist to assess any complications, monitor the device's functioning, and make any changes in its settings.
You will be mentally aware that a device is under your skin, but in most cases, it will not cause any discomfort. Our healthcare provider will provide full post-procedure guidance regarding what sensations to expect and when to seek medical attention if you experience any unusual symptoms.
Life after the CRT procedure varies from person to person, but most people experience the following benefits:
- Improvement in the symptoms related to heart failure
- Improved exercise tolerance
- Reduced hospitalization
- Enhanced cardiac function
- Improved quality of life
- Improved functional capacity
Though this procedure is safe, it can cause some risks, depending on the type of device used and your overall health. These are:
- Infection
- Bleeding, swelling or bruising at the area of insertion
- Reaction to anaesthesia
- Heart rhythm problems
- Failure of the device
- Collapsed lung
- Lead dislodgement
- Movement of the device parts that may require another surgery to correct
- Hole in the heart chamber
- Worsening of kidney function
Our cardiologists will discuss all these risks with you before the procedure and make all efforts to minimise them, providing better treatment outcomes.
Home Broadway Specialities Cardiology Cardiac-resynchronization-therapy-crt-and-crtd-implantation-2

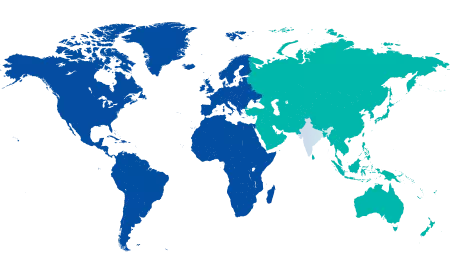
You’re on Our Indian Website
Visit the Global site for International patient services











