-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Epilepsy Clinic
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Heart Care Clinic
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physical Medicine and Rehabilitation
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Broadway
- International Patients



Clinics








- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Deep Vein Thrombosis
Deep Vein Thrombosis Treatment in Broadway
When a blood clot forms in one of the body's deep veins, it is known as deep vein thrombosis or DVT. This may occur if a vein sustains damage or blood flow is interrupted or ceases entirely. A lower-body injury and surgery involving the hips or legs are two of the most common risk factors for developing deep vein thrombosis (DVT).
DVTs can have detrimental effects. If a blood clot breaks free, it may move through the system and obstruct blood flow to the lungs. This problem, known as pulmonary embolism, is uncommon but can be lethal. A blood clot may permanently harm the vein's valves, even if it does not break free. Long-term issues with the leg, such as discomfort, swelling, and blisters, may result from this damage.
FAQ's
A pulmonary embolism is a serious DVT consequence. If a blood clot travels to your lungs and obstructs a blood vessel, you may experience a pulmonary embolism. Your lungs and other body organs may suffer severe harm due to this. If you exhibit any pulmonary embolism symptoms, get medical attention right away. These indicators consist of a vertigo-like ache in the chest that worsens when you cough or breathe deeply and quickly. Spitting blood and having a fast heartbeat.
Approximately 30% of individuals with deep vein thrombosis (DVT) may not display any noticeable symptoms. DVT commonly occurs in the veins of the arms or legs. While the symptoms can be mild, they may include:
-
A sudden enlargement of the arm or leg
-
Tenderness or pain in the arm or leg, particularly when walking or standing
-
The swollen leg appears warm to the touch and causes discomfort
-
Skin that is red or discoloured
-
Larger veins close to the skin's surface
-
Pain in the flanks or abdomen (if it affects the deep abdominal veins)
-
Seizures or severe headaches (if they impact the brain veins)
If the clot travels to the lung, pulmonary embolism symptoms include
-
Shortness of breath, a bloody cough, and chest pain.
-
Feeling dizzy or faint.
-
If you experience any symptoms, get medical help right away to prevent the consequences.
Several factors can affect venous return in the deep veins and increase the risk of blood clot formation. These factors include
-
Ageing
-
History of pulmonary embolism or DVT
-
Being diagnosed with cancer
-
Having venous conditions, such as varicose veins
-
Smoking
-
Using hormone therapy or birth control pills
-
Pregnant
-
Obese or overweight
-
Inherited blood-clotting condition
-
Fractured hips or legs, as well as extensive surgical procedures involving the hip, knee, or lower leg, can disrupt normal blood flow and clotting.
Blood clots in veins, commonly known as deep vein thrombosis (DVT), often occur in orthopaedic cases due to three primary factors: impaired veins, poor blood flow, and hypercoagulation (an increased tendency for blood to clot).
During a visit, your doctor will check for signs of DVT by examining your legs and asking you about your symptoms. They will look for changes in your skin colour, discomfort, or swelling. Depending on the determined DVT risk, tests could consist of:
-
D-dimer blood test: Helps rule out pulmonary embolism by detecting high D-dimer protein levels from blood clots
-
Duplex ultrasound: A noninvasive test for diagnosing deep vein thrombosis (DVT) that uses sound waves to create images of blood flow
-
Venography: is an invasive and uncommon medical procedure that uses dye and X-rays to visualise veins in the legs
-
MRI scan: Used to identify DVT in the veins of the abdomen
If DVT is suspected, prompt medical intervention is necessary.
Making little lifestyle adjustments could help reduce your chances of acquiring one. To maintain proper blood circulation, try these easy tips:
-
Attend to your own needs. Give up smoking, attempt to decrease your weight, and get more exercise.
-
Make routine checkups. Additionally, follow your doctor's instructions if they involve taking medication to manage a health issue.
-
Avoid prolonged sitting. Take pauses during a four-hour or longer trip to stretch and flex your lower leg muscles. If you're flying, take a stroll along the aisle every hour. When travelling long distances, stop and stretch at least every two hours. Make sure your clothing fits comfortably, and stay hydrated.
Deep vein thrombosis (DVT) treatment methods include:
-
Anticoagulants: Blood thinners that stop the formation of new clots, such as rivaroxaban, warfarin, and heparin
-
Thrombolytics: Medicines that dissolve clots, such as alteplase, for pulmonary embolism or severe DVT
-
Compression Stockings: Minimise oedema
-
Inferior Vena Cava (IVC) Filter: When anticoagulants are not appropriate, this filter is inserted into a big vein to capture clots
-
Lifting the Afflicted Limb: Assists in minimising discomfort and swelling
-
Lifestyle Modifications: To avoid recurrence, maintain a healthy weight, stop smoking, and engage in regular exercise
-
Monitoring and Follow-up: Periodic evaluations to oversee and modify treatment plans
You can take specific measures to aid in your deep vein thrombosis (DVT) recovery.
Upon discharge from the hospital, you will be recommended to:
-
Walk regularly
-
Delay taking any flights or lengthy trips for at least two weeks after starting blood thinner medication.
-
Keep your affected leg elevated when you're seated.
Home Broadway Specialities Radiology Deep-vein-thrombosis-2

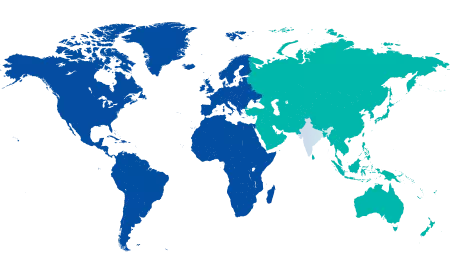
You’re on Our Indian Website
Visit the Global site for International patient services











