-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Epilepsy Clinic
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Heart Care Clinic
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physical Medicine and Rehabilitation
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Renal Sciences
- Rheumatology
- Surgical Gastro
- Surgical Oncology
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Broadway
- International Patients



Clinics








- Self Registration
- In-Patient Deposit
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Lap LAR and Ileostomy
Lap LAR and Ileostomy Procedure in Broadway
This advanced, minimally invasive surgery is designed to treat complex conditions of the lower colon, including rectal cancer. By using small incisions in the abdomen, our skilled surgeons can remove the affected portion of the rectum while preserving sphincter function, which helps maintain normal bowel control. This approach offers numerous benefits over traditional open surgery, including reduced postoperative pain, shorter hospital stays, faster recovery, and improved cosmetic results due to the use of specialised instruments and a laparoscope for enhanced visualisation.
Ileostomy
An Ileostomy is a surgical procedure that creates an opening (stoma) in the abdominal wall, allowing the ileum (a part of the small intestine) to be brought to the surface. This procedure is typically performed when the colon and rectum need to be removed or bypassed due to conditions such as cancer, trauma, or inflammatory bowel disease. The waste is collected in an external pouch or ostomy bag. Depending on the patient's condition and recovery needs, an Ileostomy may be temporary or permanent.
Both Lap LAR and Ileostomy represent significant advancements in colorectal surgery, offering personalised treatment options that enhance patient outcomes and quality of life. Our team at Manipal Hospitals, the best Ileostomy treatment hospital in Broadway, is committed to providing the highest level of care with these sophisticated techniques to ensure the best possible results for our patients.
FAQ's
The main indications for Laparoscopic Low Anterior Resection are benign disorders such as big rectal polyps or strictures that need to be removed, as well as rectal cancer, particularly in the mid-to-lower rectum. It is appropriate for patients with favourable health profiles and circumscribed rectal malignancies because it attempts to maintain the function of the anal sphincter. Benefits from Lap LAR include less pain, quicker healing, shorter hospital stays, and better aesthetics; they are especially alluring to those who prefer less invasive procedures.
Compared to open surgery, Laparoscopic Low Anterior Resections, or Lap LARs, have fewer side effects, less pain following surgery, faster recovery and an earlier return of bowel function, shorter hospital stays, better cosmetic results, and possibly fewer rates of wound infections and hernias. For many patients undergoing colorectal surgery, Lap LAR is the preferred procedure despite possible concerns such as extended operating durations and difficulties linked to pneumoperitoneum, particularly when carried out by skilled surgeons in specialised facilities.
The steps involved in Laparoscopic Low Anterior Resection (Lap LAR) are trocar insertion, pneumoperitoneum creation, and patient positioning. During the procedure, the surgeon makes several small incisions in your abdomen. A special camera and tools are inserted through these tiny cuts to view and work inside your belly. The surgeon carefully removes the affected part of the rectum while preserving as much of the healthy tissue as possible. After removing the diseased section, the remaining parts of the colon and rectum are stitched back together. The small incisions are then closed.
For patients with rectal cancer, factors such as tumour characteristics (such as size and stage), patient anatomy (including previous surgeries and body type), medical history (including comorbidities), surgeon expertise, patient preferences (such as preference for minimally invasive surgery), and the risks of complications associated with each approach all play a role in the decision between Laparoscopic Low Anterior Resection (Lap LAR) and open surgery. The best course of treatment is selected in collaboration with these variables, taking into account each patient's needs and desired results.
For rectal cancer, Laparoscopic Low Anterior Resection, or Lap LAR, produces oncological results that are comparable to those of open surgery, such as sufficient tumour clearance, lymph node retrieval, overall survival, disease-free survival, and rates of local recurrence. Furthermore, Lap LAR has advantages like less pain following surgery, a quicker recovery, and better cosmetic outcomes, all of which may improve patients' quality of life. For rectal cancer, Lap LAR is often a safe and efficient treatment option with good oncological and patient-centred outcomes.
In surgical gastroenterology, an Ileostomy is advised to temporarily or permanently redirect faecal flow, promoting recovery following procedures such as those for colon cancer or inflammatory bowel disease. It treats emergencies like obstructions or perforations, eases bowel rest situations brought on by inflammation or infection, and enhances nutrition when malabsorption occurs. Recommendations are based on the health, preferences, and goals of the patient's treatment, with the ultimate goal of effectively improving quality of life and gastrointestinal function.
In situations such as flare-ups of inflammatory bowel disease or following trauma, temporary Ileostomies are used to temporarily redirect faecal flow from damaged intestine segments in order to promote recovery. Since they are reversible, stoma care and careful observation are necessary to ensure healing preparedness. Permanent Ileostomies, on the other hand, are permanent fixes for non-reconstructable intestines brought on by conditions like Crohn's or by after-effects like fistulas. They require ongoing stoma care, assistance for lifestyle modifications linked to long-term stoma management, and adaptability.
To stay hydrated and avoid difficulties, patients adjusting to life with an Ileostomy must manage physical modifications such as stoma care and nutritional control. Adapting to shifts in body image and looking for assistance to boost self-esteem are examples of emotional issues that need to be dealt with following surgery. Developing everyday activities and stoma care regimens are practical concerns. In the long run, patients prioritise improving their quality of life by continuing their education and adjusting to new technologies. Peer and healthcare provider support is essential for a successful transition and the maintenance of a healthy lifestyle.
Home Broadway Specialities Surgical-gastro Lap-lar-and-ileostomy

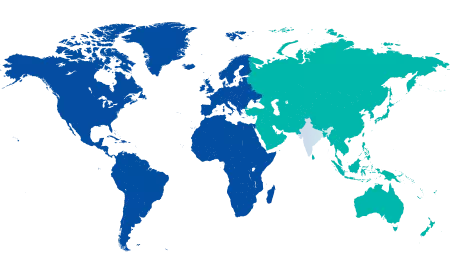
You’re on Our Indian Website
Visit the Global site for International patient services











