
Cervical cancer remains one of the most common gynaecological cancers worldwide, posing a significant threat to women's health. Despite the availability of effective surgical options and a long precancerous phase, the disease continues to be a leading cause of cancer-related deaths among women. This is often due to a lack of awareness and inconsistencies in screening measures. However, with the World Health Organization's (WHO) goals for 2030, there is hope for a significant reduction in the burden of cervical cancer through primary prevention, effective cervical cancer screening tests, and timely treatment.
AI-inspired by the structure and function of the human brain—utilizes deep learning models like Convolutional Neural Networks (CNNs) to process and analyze complex data. One of the most promising advancements in this field is the integration of AI into medical diagnostics, such as improving cervical cancer screening methods for more efficient and accurate early detection and prevention.
Synopsis
The Role of AI in Cervical Cancer Detection
AI Technology
AI technologies, particularly machine learning and deep learning, have revolutionized various aspects of medical diagnostics. In cervical cancer screening tests, AI can be utilized in several ways:
-
Automated Visual Evaluation (AVE): AVE uses AI to analyze visual images of the cervix, reducing the subjectivity and variability associated with human interpretation. This method can significantly enhance the accuracy of visual inspections, making it a valuable tool in resource-limited settings.
-
Computer-Assisted Reading of Pap Smears: AI algorithms can assist in the interpretation of Pap smears, identifying abnormal cells with high precision. This not only speeds up the diagnostic process but also reduces the workload on cytotechnicians, who are often in short supply.
-
HPV Testing: Human papillomavirus (HPV) is the primary cause of cervical cancer. AI can improve the accuracy of HPV testing by analyzing test results and identifying high-risk cases that require further investigation.
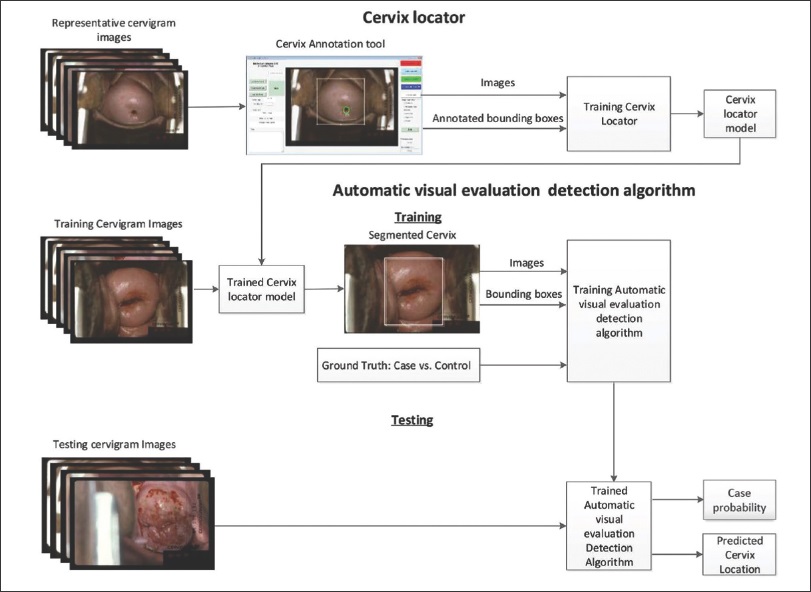
The Process of Automated Visual Evaluation
For successful AVE, it is crucial to differentiate between low-grade squamous intraepithelial lesions (LSIL), which can often resolve without treatment, and high-grade squamous intraepithelial lesions (HSIL), which require immediate evaluation and treatment. The process involves training a convolutional neural network (CNN) to distinguish between these two types of epithelial appearances within the transformation zone of the cervix.
-
Training the Model: The first step is to expose the CNN to a large series of cervical images with known severity, supported by histopathology. The model extracts high-level features such as edges, colour, and gradient orientation to form a network between the convoluted layers.
-
Categorization: The CNN categorizes cervical images into one of two categories (≤LSIL or HSIL) by outputting the probability that a given image belongs to either category. This involves two steps: the training set and the validation set.
-
Validation: During training, the CNN adjusts its parameters to minimize the error between its predictions and the ground truth. The model's performance is then evaluated using a validation set, which does not include images from the training set. This ensures the model's generalizability to predict cervical disease.
Comparing Traditional Methods and AI-Driven Approaches
|
Aspect |
Traditional Methods |
AI-Driven Approaches |
|
Accuracy |
Relies heavily on human interpretation, prone to variability and subjectivity. |
High precision and consistency using advanced machine learning algorithms like Convolutional Neural Networks. |
|
Cost |
Often cost-effective but requires frequent re-evaluations due to lower accuracy in some cases. |
Initial investment is high, but long-term savings through efficient and accurate diagnostics. |
|
Human Resources |
Requires trained cytotechnicians and pathologists, leading to workload issues in resource-limited settings. |
Reduces reliance on human expertise, addressing shortages of skilled professionals in low-resource areas. |
|
Scalability |
Limited scalability in resource-poor regions due to infrastructure and workforce constraints. |
Highly scalable and deployable in remote areas with AI-enabled portable devices like the Mobile ODT EVA system. |
|
Detection Sensitivity |
Lower sensitivity in distinguishing low-grade and high-grade lesions, leading to potential underdiagnosis. |
High sensitivity and specificity in identifying precancerous and cancerous lesions, even at early stages. |
|
Data Utilization |
Minimal use of historical data for improving diagnostics. |
Learns and improves from vast datasets, ensuring continuous advancements in accuracy and efficiency. |
Promising Results and Challenges
Many machine learning-based approaches have shown promising results in cervical cancer screening. For instance, a study by Song et al. in 2015 achieved 74% sensitivity and 90% specificity in differentiating high-grade cervical lesions from low-grade lesions and normal tissue using a data-driven computer algorithm.
In a population-based longitudinal cohort study using faster region-based CNN (Faster R-CNN) involving 9406 women in Costa Rica, the algorithm demonstrated high accuracy in identifying cervical precancers. The AVE of cervigrams collected at enrollment identified cases of precancer or cancer with greater accuracy than the interpretation by a colposcopist or conventional cytology.
Technological Advancements for Gynecologic Cancer Treatment
Gynecologist Appointment
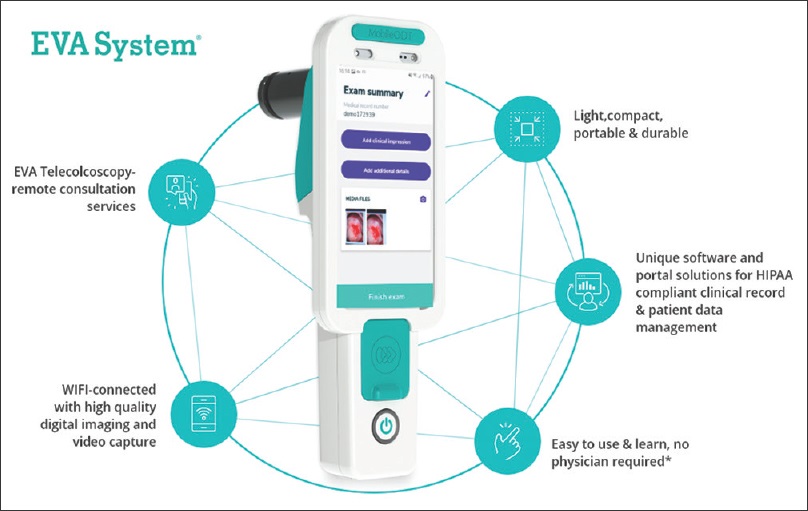
An integral part of AVE is image capture, and significant advancements have been made in this area. The Mobile ODT EVA system, for example, uses a smartphone camera coupled with a cross-polarized light source, an external magnifying lens, and an application to assist image capture and data communication. This system has demonstrated its utility in enhancing the accuracy of visual inspections.
Consult our gynaec oncologist in Delhi if you need treatment and care for cervical cancer
Current Scenario and Future Directions
The main burden of gynaecological cancer lies in areas with a lack of trained healthcare personnel and limited equipment. Frequent hospital visits, underdiagnosis of precancerous lesions, and loss of follow-up can undermine efforts to combat this disease. Automated detection, computing, and analysis can improve the accuracy of screening and overcome time constraints.
However, there are challenges to the widespread adoption of AI in cervical cancer screening. One major drawback is the acquisition of data, as millions of observations are required to achieve acceptable performance levels. Additionally, the integration of AI into existing healthcare systems requires significant investment in technology and training.
Despite these challenges, the potential benefits of AI in gynecologic cancer surgery are immense. By bridging the gap between medicine and technology, AI can provide accurate and efficient screening solutions, even in remote and resource-limited areas. This can lead to earlier detection, timely treatment, and ultimately, a reduction in cervical cancer incidence and mortality.
Conclusion
The future of cervical cancer screening lies in the effective integration of AI into healthcare systems. As AI technologies continue to evolve, they will become more accessible and affordable, making them available to a broader population. The development of indigenous vaccines and AI-based screening tools can further enhance the coverage and effectiveness of cervical cancer prevention programs.
In conclusion, AI has the potential to revolutionize cervical cancer screening, offering a more accurate, efficient, and accessible approach to early detection and prevention. By leveraging the power of AI, we can move closer to the WHO's goal of significantly reducing the burden of cervical cancer by 2030, ensuring better health outcomes for women worldwide.
However, with efforts like those highlighted on World Cancer Day, the focus on awareness, prevention, and innovation brings us closer to reducing cervical cancer mortality.
Explore the Future of Healthcare at Manipal
Manipal is at the forefront of integrating cutting-edge technologies like AI into healthcare. With a commitment to innovation and excellence, Manipal is dedicated to improving health outcomes and advancing medical research. Join us in our mission to harness the power of AI for a healthier future.
FAQ's
AI enhances cervical cancer screening by utilizing advanced machine learning and deep learning models. These models can assist in automated visual evaluation (AVE), HPV testing, and computer-assisted Pap smear reading, allowing for faster and more accurate identification of abnormal cells and precancerous lesions, ultimately leading to earlier detection and treatment.
The key benefits of using AI in cervical cancer detection include increased accuracy, efficiency, and accessibility. AI reduces human error, speeds up the diagnostic process, and provides reliable results, especially in resource-limited settings where access to skilled professionals may be limited.
No, AI is not meant to replace doctors. Instead, it acts as a tool to assist healthcare professionals in providing more accurate and efficient diagnoses. It can help reduce the workload of cytotechnicians, enhance the interpretation of Pap smears, and assist in visual evaluations, but doctors are still essential for clinical decision-making and patient care.
Automated Visual Evaluation (AVE) is an AI-driven process that uses computer algorithms to analyze images of the cervix. AVE helps detect precancerous lesions by distinguishing between low-grade and high-grade lesions, improving the accuracy of visual inspections and helping to identify cases that need further medical attention.
While AI shows great promise, some challenges remain, such as the acquisition of sufficient data for training AI models, which requires millions of observations. Additionally, integrating AI into existing healthcare systems may require substantial investment in technology and training, especially in under-resourced areas. Despite these hurdles, AI offers substantial potential to improve screening accuracy and efficiency.



















 7 Min Read
7 Min Read

















