
Imagine your body as a well-oiled machine, running smoothly with every function in perfect sync. Now, picture a crucial filter breaking down, allowing harmful toxins to build up and fluids to overflow. This is what happens when the kidneys fail. These vital organs work tirelessly, filtering waste, balancing electrolytes, and ensuring fluid levels remain optimal. But when they can no longer perform their job, dialysis steps in as a life-saving substitute.
This blog explores the necessity of dialysis, the different types available, and what patients can expect from this procedure.
Synopsis
When is Dialysis Necessary?
Dialysis is required when the kidneys lose their ability to function adequately, typically when their function declines to 10-15% of normal capacity. This condition is commonly referred to as end-stage renal disease (ESRD). Several factors contribute to this decline, including:
-
Chronic Kidney Disease (CKD): A progressive condition often caused by diabetes or hypertension.
-
Acute Kidney Injury (AKI): Sudden kidney failure due to severe illness, injury, or toxic exposure.
-
Polycystic Kidney Disease (PKD): A genetic disorder leading to the growth of fluid-filled cysts in the kidneys.
-
Glomerulonephritis: An inflammatory disease that damages the kidney's filtering units.
-
Severe Infections or Autoimmune Diseases: Conditions like lupus can cause long-term kidney damage.
Patients with ESRD experience symptoms like fluid retention, electrolyte imbalances, extreme fatigue, and toxin buildup in the blood. Dialysis helps replace lost kidney function and alleviate these symptoms.
|
Signs You May Need Dialysis |
Why It Happens |
|
Swelling in legs, feet, or face |
Kidneys can't remove excess fluid |
|
Fatigue and weakness |
Buildup of toxins in the blood |
|
Nausea and vomiting |
Waste accumulation in the body |
|
Fluid overload affecting the lungs |
|
|
Confusion or difficulty concentrating |
Toxin buildup affecting brain function |
Types of Dialysis
There are two main types of dialysis—hemodialysis and peritoneal dialysis, each with specific variations. Understanding these types can help patients and caregivers choose the best option.
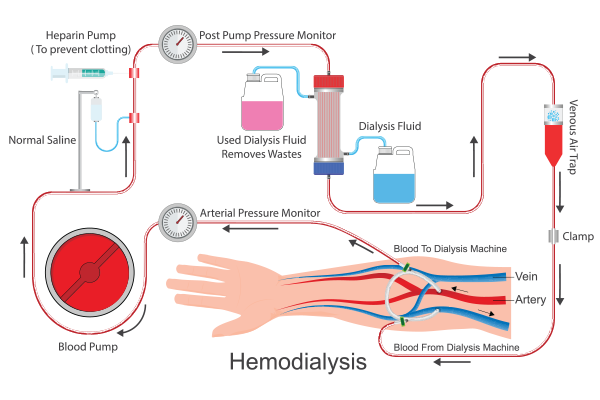
Hemodialysis (HD)
This is the most common type of dialysis, where blood is drawn from the body, filtered through a dialyzer (artificial kidney), and then returned to the body. There are three types of hemodialysis:
-
In-Center Hemodialysis: Conducted at a dialysis center, usually three times a week for 3-5 hours per session.
-
Home Hemodialysis (HHD): Allows patients to perform dialysis at home with proper training and equipment.
-
Nocturnal Hemodialysis: Longer and slower dialysis performed overnight, leading to better toxin removal and fewer side effects.
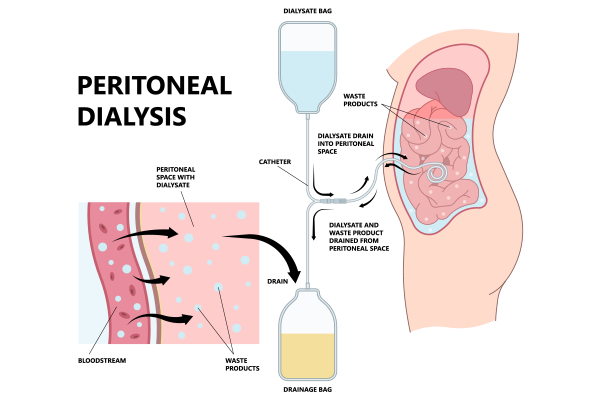
Peritoneal Dialysis (PD)
Peritoneal dialysis uses the body's peritoneal membrane inside the abdomen as a natural filter. There are two primary types:
-
Continuous Ambulatory Peritoneal Dialysis (CAPD): Performed manually throughout the day without a machine.
-
Automated Peritoneal Dialysis (APD): Uses a machine (cycler) to perform exchanges overnight while the patient sleeps.
Dialysis Procedure Explained
Hemodialysis Process:
-
A vascular access is created, usually through an arteriovenous (AV) fistula, graft, or catheter.
-
Blood is drawn from the body and passed through a dialyzer to remove toxins and excess fluids.
-
The clean blood is returned to the body.
-
Each session lasts 3-5 hours and is usually done three times a week.
Peritoneal Dialysis Process:
-
A catheter is placed into the abdominal cavity.
-
A dialysis solution is introduced into the peritoneal cavity, allowing waste and excess fluid to be drawn out.
-
After a set dwell time, the fluid is drained and replaced with fresh dialysis fluid.
-
This process can be done manually (CAPD) or through a machine (APD).
|
Difference between |
Hemodialysis |
Peritoneal Dialysis |
|
Performed at home or center? |
Usually in a center, but can be done at home |
Mostly at home |
|
Frequency of treatment |
3-4 times per week |
Done daily |
|
Equipment required |
Dialysis machine and dialyzer |
Catheter and dialysis fluid |
|
Major risk |
Low blood pressure, infections at access site |
Infection (peritonitis) |
|
Suitable for an active lifestyle? |
Limited flexibility due to scheduled sessions |
More flexibility |
More Reads: Kidney Transplant - When is it needed?
Is Dialysis Uncomfortable?
A common concern among patients is whether the process is painful. The procedure itself is generally not painful, but there may be discomfort due to:
-
Needle insertion for hemodialysis.
-
Abdominal bloating and mild discomfort during peritoneal dialysis.
-
Cramps or low blood pressure due to fluid removal.
These issues can usually be managed with proper medical guidance and lifestyle adjustments.
Risks and Benefits of Dialysis
Benefits:
-
Removes waste and excess fluids, preventing complications.
-
Improves overall well-being and reduces symptoms of kidney failure.
-
Allows patients to continue leading an active life.
Risks:
-
Infection risk at the access site.
-
Low blood pressure during hemodialysis.
-
Hernias and bloating in peritoneal dialysis.
-
Long-term cardiovascular strain.
While dialysis is a life-sustaining treatment, kidney transplantation remains the preferred long-term solution for eligible patients.
World Kidney Day Message & Expert Nephrology Care at Manipal Hospital Dwarka
On World Kidney Day, let's take a moment to recognize the importance of kidney health and early detection. Kidneys are vital for overall well-being, and taking proactive steps—like maintaining a balanced diet, staying hydrated, and managing blood pressure—can help prevent kidney disease. Regular checkups and early intervention are key to avoiding dialysis and ensuring a healthy life.
For world-class kidney care, Manipal Hospital Dwarka offers the best treatment options for highly skilled nephrology teams. If you or a loved one require dialysis or kidney care, trust Manipal Hospital Dwarka for excellence in nephrology treatment. Schedule a consultation today and take a step toward better kidney health!
FAQ's
Dialysis mimics kidney function but does not fully replace the kidneys' ability to regulate hormones and blood pressure.
With proper care, patients can live for decades on dialysis, though kidney transplantation often offers a better quality of life.
Yes, but they need to coordinate with dialysis centers at their destination.
Yes, they should manage potassium, sodium, phosphorus, and fluid intake to avoid complications.
Yes, when feasible, a kidney transplant offers greater freedom and a higher life expectancy compared to long-term dialysis.



















 5 Min Read
5 Min Read












