
Blood cancers, such as leukaemia, lymphoma, and multiple myeloma, present unique and often complex challenges in oncology. Thankfully, the treatment landscape has dramatically evolved, offering hope for many patients. Among the most groundbreaking advancements are Bone Marrow Transplant (BMT) and Chimeric Antigen Receptor T-cell (CAR-T cell therapy).
These innovative therapies represent the future of blood cancer treatment, harnessing the power of the body's immune system and regenerative capabilities to tackle these life-threatening conditions. Let’s dive deeper into these therapies, how they work, and their transformative potential.
Synopsis
Bone Marrow Transplant (BMT): A Lifeline for Many
What is BMT?
Bone Marrow Transplant, or hematopoietic stem cell transplant, involves replacing damaged or diseased bone marrow with healthy stem cells. These stem cells, which can be sourced either from the patient (autologous transplant) or a compatible donor (allogeneic transplant), are responsible for generating healthy blood cells and rejuvenating the immune system.
How Does BMT Work?
BMT begins with intensive chemotherapy or radiation therapy to destroy the patient’s unhealthy bone marrow. Following this, healthy stem cells are introduced into the body, where they migrate to the bone marrow and start the process of blood cell regeneration. This reboot of the bone marrow can potentially cure many patients, particularly those with relapsed or high-risk blood cancers.
Types of BMT
-
Autologous Transplant: The patients who have achieved disease remission, their stem cells are harvested, treated, and reintroduced after therapy. This is typically used for multiple myeloma and certain lymphomas.
-
Allogeneic Transplant: Stem cells are obtained from a donor, which can be a sibling, an unrelated donor, or even umbilical cord blood. This is the preferred approach for leukaemia and other aggressive blood cancers.
Benefits and Risks
BMT offers the potential for a cure in many patients. However, it’s not without risks. Complications like graft-versus-host disease (GVHD), infections, and organ damage can arise. The good news is that improved techniques in matching donors and advancements in supportive care have significantly reduced these risks.
CAR-T Cell Therapy: Revolutionizing Immunotherapy
What is CAR-T Cell Therapy?
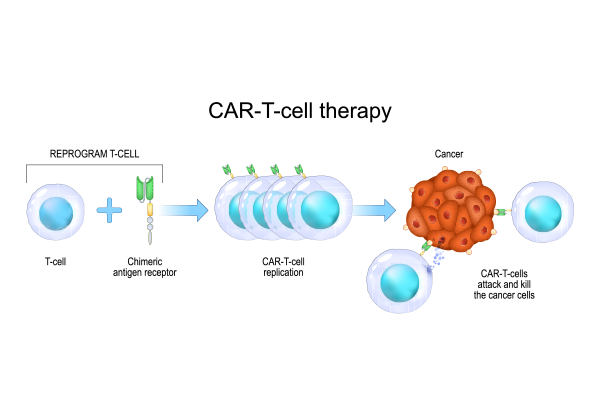
CAR-T cell therapy is an advanced form of immunotherapy where a patient’s T cells are genetically engineered to target and attack cancer cells. This therapy is a game-changer because it unleashes the power of the immune system to directly combat cancer in a personalized way.
How Does CAR-T Work?
The treatment starts with the collection of T cells from the patient’s blood. In the lab, these T cells are altered to express chimeric antigen receptors (CARs) that can identify cancer cells. After the modified T cells are multiplied, they’re infused back into the patient. Once inside the body, the CAR-T cells seek out cancer cells by recognizing specific markers, destroying them in the process.
Applications of CAR-T Therapy
CAR-T therapy has shown remarkable success, particularly in the treatment of cancers that resist traditional therapies. It is currently FDA-approved for:
-
Acute Lymphoblastic Leukemia (ALL): Especially beneficial for children and young adults.
-
Diffuse Large B-cell Lymphoma (DLBCL): A major form of non-Hodgkin lymphoma.
-
Multiple Myeloma: A promising treatment for relapsed or refractory cases.
Benefits and Challenges
CAR-T cell therapy is incredibly effective, offering the possibility of long-term remission and even a cure. However, the treatment can trigger side effects like cytokine release syndrome (CRS) and neurotoxicity. Furthermore, it comes at a high financial cost. However, ongoing research is focusing on enhancing the therapy’s safety, effectiveness, and cost-effectiveness.
Looking to the Future: What’s Next in Blood Cancer Treatment?

The field of blood cancer treatment is evolving rapidly, with several exciting developments on the horizon.
Combination Therapies: Synergy in Action
Researchers are exploring the possibility of combining BMT with CAR-T cell therapy to improve outcomes. For example, CAR-T cells might be used to prevent relapse following a BMT or as a bridge to the transplant itself.
Universal CAR-T Cells: The Future of Treatment Accessibility
One of the most promising breakthroughs is the development of “universal” CAR-T cells. These off-the-shelf cells can be used for any patient, bypassing the need for individualized cell manufacturing. This could drastically reduce costs and make this life-saving treatment more widely available.
Gene Editing and Precision Medicine: The Next Frontier
Technologies like CRISPR are being employed to further fine-tune CAR-T cell therapy, making it even more precise and effective. Additionally, precision medicine approaches are emerging, which tailor treatments based on the genetic makeup of both the patient’s cancer and their overall health.
Expanding Applications: From Blood to Solid Tumors
While CAR-T therapy has already proven effective for certain blood cancers, researchers are working to extend its benefits to other types of blood cancers and even solid tumours like breast and lung cancer. Early-stage clinical trials are already underway to test this.
Conclusion: A New Era for Blood Cancer Patients
The future of blood cancer treatment is bright. With advancements like Bone Marrow Transplantation and CAR-T cell therapy, patients now have access to therapies that offer both hope and long-term survival. Despite the challenges these treatments may pose, ongoing research is pushing the boundaries of what’s possible.
For patients seeking cutting-edge care, Manipal Hospitals Dwarka stands at the forefront of innovative cancer treatments. With state-of-the-art technology and a dedicated team of oncologists, Manipal Hospitals Dwarka offers patients access to the latest therapies for blood cancers, ensuring that each patient receives the most effective, personalized treatment available with a top Bone Marrow Specialist in Delhi.
By staying informed about the latest breakthroughs and continuing to support cancer research, we can look forward to a future where blood cancers are no longer a death sentence, but a treatable condition.
FAQ's
BMT replaces damaged bone marrow with healthy stem cells, while CAR-T therapy modifies a patient's T cells to target cancer cells. BMT is used for cancers like leukaemia and lymphoma, while CAR-T is often for cancers resistant to traditional treatments.
CAR-T therapy has shown high success rates, especially for relapsed or refractory cancers like ALL and lymphoma. It can lead to long-term remission but comes with risks like cytokine release syndrome and neurotoxicity.
Risks include graft-versus-host disease (GVHD), infections, and organ damage. However, improved donor matching and supportive care have reduced these risks over time.
Currently, CAR-T therapy is most effective for blood cancers, but research is ongoing to expand its use to solid tumours like breast and lung cancers.
Both treatments are expensive, with costs ranging from tens of thousands to several hundred thousand dollars. Insurance and clinical trials may help reduce the financial burden.



















 5 Min Read
5 Min Read















