Have you ever felt short of breath, even when doing simple tasks? This could be a sign of Interstitial Lung Disease (ILD) or lung disease fibrosis. This condition affects the lungs' tiny air sacs, making it harder to breathe.
Interstitial Lung Disease (ILD) is a group of lung conditions that cause scarring (fibrosis) in the lungs. This scarring makes it hard to breathe and get enough oxygen into the bloodstream. It affects the tissue and space around the air sacs of the lungs. If not treated early, ILD can lead to severe lung problems, including lung fibrosis and bronchiectasis disease.
But how do you know if you or someone you love might have this condition? What tests can doctors diagnose, and what treatments are available? Let's break it down.
Synopsis
What is Interstitial Lung Disease?
Interstitial Lung Disease (ILD) refers to a group of over 200 lung conditions that cause lung tissue inflammation and scarring (fibrosis). This scarring affects the spaces around the air sacs in the lungs, making it harder for oxygen to pass into the bloodstream. The most common forms include:
-
Pulmonary Fibrosis: This happens when the lung tissue becomes thick and scarred.
-
Interstitial Lung Pneumonia: This is an inflammation in the lungs that causes similar scarring in the lung.
What are the Causes and Symptoms?
While the exact cause is often unknown, ILD can result from long-term exposure to harmful substances. Some possible causes include:
-
Autoimmune diseases such as rheumatoid arthritis, systemic sclerosis or lupus.
-
Long-term exposure to harmful substances like asbestos, coal dust, or mould.
-
Exposure to pigeons and pigeon droppings
-
Certain medications that affect the lungs, such as chemotherapy drugs.
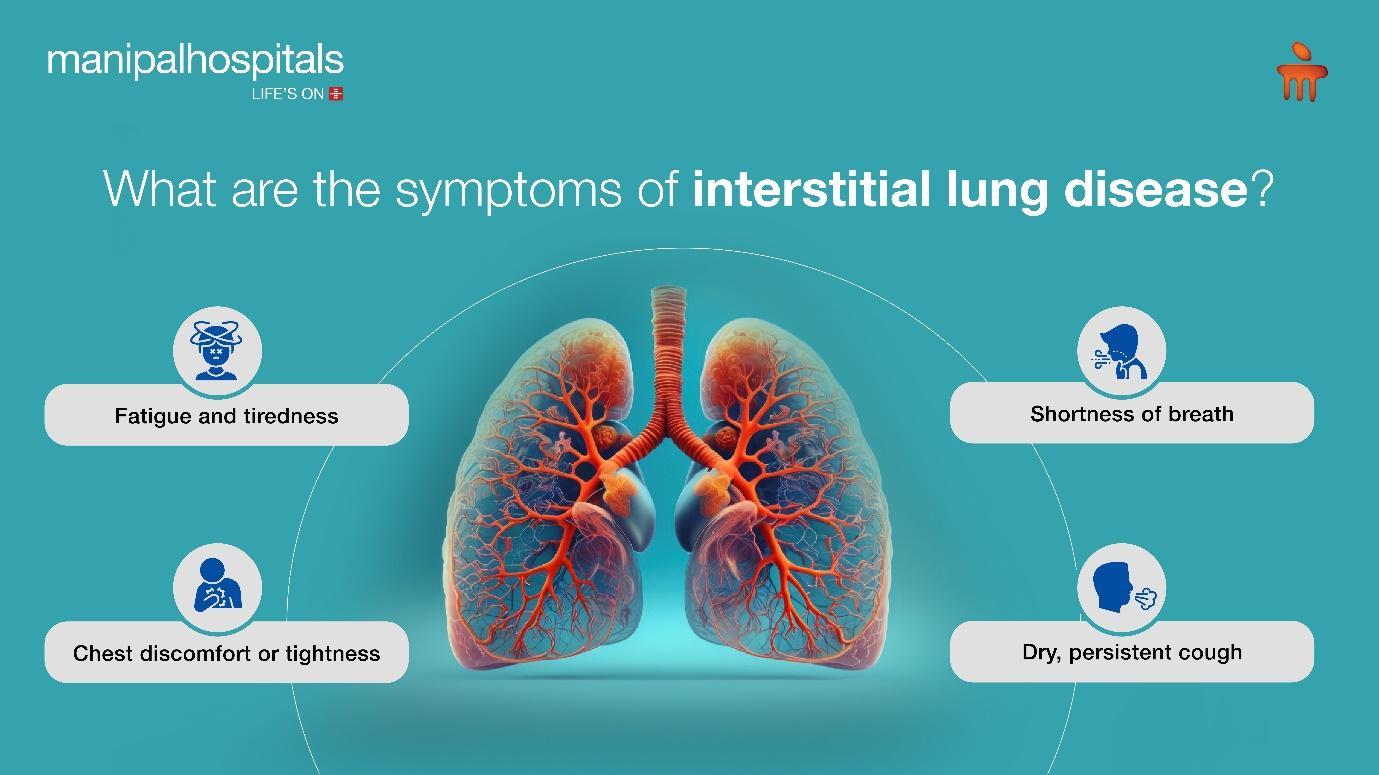
Key symptoms of interstitial lung disease are:
Lung infection symptoms can sometimes resemble other common conditions, making ILD hard to identify early. Some of the potential symptoms are as follows:
-
Shortness of breath, especially during or after physical activity
-
Dry, persistent cough
-
Fatigue and tiredness
-
Chest discomfort or tightness
What Happens When You Have ILD?
When you have interstitial lung disease or ILD, your lung tissues will get damaged. Over time, the lungs will start to become stiff and less able to expand. This reduces the amount of oxygen that enters the bloodstream. As the disease progresses, breathing can become more difficult, leading to low oxygen levels and damage to other organs. The scarring is usually irreversible, so early diagnosis and treatment are important to slow the progression of lung fibrosis.
When to Suspect Interstitial Lung Disease?
You might suspect ILD if you experience persistent lung infection symptoms or breathing problems that don’t go away. If you have a history of exposure to harmful lung irritants, are a smoker, are over 70 years of age, or have an autoimmune condition, you could be at greater risk. If you notice any unusual breathing difficulties, it is advised to see your doctor.
How is Interstitial Lung Disease Diagnosed?
When a doctor suspects ILD, they will typically start with a physical exam and a detailed medical history. Several tests help confirm the diagnosis:
-
Chest X-ray: It helps to see shadows or scarring in the lungs.
-
High-resolution CT scan: It provides detailed images to assess the severity of lung fibrosis.
-
Pulmonary function tests (PFTs): Measure how well your lungs are working by checking airflow and oxygen levels.
-
Bronchoscopy: A small camera is inserted into the airways to examine the lung tissue.
-
Lung biopsy: Takes a small sample of lung tissue for closer examination.
Treatment Options for Interstitial Lung Disease
While there is no cure for ILD, treatments focus on managing symptoms and slowing disease progression. The interstitial lung disease treatment plan will depend on the specific type of ILD and its severity. Common treatments include:
-
Medications: Anti-inflammatory drugs and immunosuppressants can help reduce lung inflammation and slow scarring.
-
Antifibrotic drugs don’t cure fibrosis but slow down the disease progression
-
Oxygen therapy: This helps patients with low blood oxygen levels breathe more comfortably.
-
Pulmonary rehabilitation: A combination of exercise, breathing techniques, and education to improve lung function.
-
Lung transplant: In severe cases, a lung transplant may be the only option for extending life.
Interstitial Lung Disease is a serious, often progressive condition that affects the lungs’ ability to function properly. Early detection is key to managing the disease and improving quality of life. If you experience symptoms like shortness of breath, a persistent cough, or chest tightness, don't wait—see your pulmonology doctor. With proper testing and treatment, patients can slow the progression of ILD and maintain better lung health.
By recognising the signs early and seeking appropriate care, you can take control of your lung health before the disease progresses.
FAQ's
Early symptoms of ILD include shortness of breath, especially during physical activity, a dry, persistent cough, fatigue, and chest discomfort.
The exact cause of ILD is often unknown. However, common triggers include long-term exposure to harmful substances like asbestos or coal dust, autoimmune diseases such as rheumatoid arthritis, and certain medications, including chemotherapy drugs.
Generally, there is no cure for ILD which has resulted in fibrosis. However, treatments are available to manage symptoms and slow the progression of lung fibrosis- medications, oxygen therapy, pulmonary rehabilitation etc.
Individuals with a history of long-term exposure to harmful substances, smokers, family history, those with autoimmune diseases, and people taking certain medications are at a higher risk of developing ILD.
The life expectancy for ILD varies depending on the specific type of ILD, its severity, and how early it is diagnosed. Some patients can live many years with the disease if properly managed.
While ILD cannot always be prevented, reducing exposure to harmful substances, not smoking, and managing underlying conditions such as autoimmune diseases can lower the risk of developing ILD.






















 4 Min Read
4 Min Read