-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Epididymitis
Epididymitis Treatment in Dhakuria
Epididymitis Treatment in Dhakuria, West Bengal
Epididymitis is a clinical syndrome present with inflammation, pain, and swelling of the epididymis, a tube that carries and stores sperm. The condition typically affects men between 14 to 35 years.
Causes of Epididymitis
- Sexually transmitted infections are a predominant cause
- Urinary tract or prostate infections
- Bacterial or viral infections
- Backward flow of urine
- Blockage in urethra
- Infected or enlarged prostate
- Use of catheter
- Groin injury caused by trauma
Epididymitis Treatment
- An Antibiotic therapy lasting for two weeks helps alleviate the problem
- Taking proper rest
- Keeping the scrotum in an elevated position
- Applying ice bags to reduce swelling and pain
- Increasing fluid intake
- Using pain relief medications
Visit Manipal Hospitals, if you experience sudden pain and swelling in your genitals.
FAQ's
The term "epididymitis" describes inflammation of the epididymis, a tightly wound tube that stores and moves sperm and is situated below the testicle. Testicular pain can range in intensity from slight discomfort to severe agony, and it is commonly caused by inflammation. The afflicted testicle may also show signs of enlargement, redness, warmth, and discomfort. Numerous conditions, including bacterial infections, STDs, urinary tract infections, or physical trauma, can cause epididymitis.
While epididymitis can strike anyone at any age, it most frequently affects people in the 14–35 age range. Men at birth are prone to acquiring epididymitis. Numerous conditions, such as bacterial infections, STDs, urinary tract infections, or physical damage to the genital area, can cause this illness. Seeking medical attention for epididymitis symptoms is crucial for an accurate diagnosis and treatment to prevent complications and ease discomfort, regardless of age or gender.
Pain in the scrotum is a common symptom of epididymitis, and it occasionally spreads to the surrounding groin area. Common symptoms include fever, chills, swelling and redness in the afflicted testicle; other possible symptoms include blood in the semen, dysuria (painful urination), and fever. The intensity of these symptoms can vary, and they can greatly interfere with day-to-day activity. Seeking medical attention is essential for an early diagnosis and suitable therapy to properly manage epididymitis and avoid complications.
The majority of epididymitis cases are caused by infections; prominent culprits include Escherichia coli (E. coli), Mycoplasma, and Chlamydia, which are frequently spread through sexual contact. Though less frequently, other infectious agents such as tuberculosis or the mumps virus can also cause epididymitis. Urinary reflux, a condition in which pee rushes backwards into the epididymis and is frequently brought on by hard lifting, can also result in epididymitis. Additional causes include surgical operations involving the prostate, urethra, or bladder, urethral blockage, catheter use, prostate problems such as hypertrophy or infection, and traumatic injuries to the groin area.
Yes, although epididymitis is not considered an STD in and of itself, it frequently presents as a sign of other STDs, including gonorrhoea and chlamydia. The spread of these infections through sexual contact can cause inflammation of the epididymis and the subsequent development of epididymitis. Thus, it is essential to have safe sexual behaviour and to contact a doctor as soon as possible if you experience any signs of an STD to avoid consequences like epididymitis.
Healthcare professionals usually physically examine the scrotum to check for soreness or swelling to diagnose epididymitis. If germs are found in the urine, it may be necessary to perform a urinalysis to rule out an underlying infection. To help confirm the diagnosis and gauge the degree of inflammation, Ultrasound imaging may occasionally be used to acquire diagnostic images of the scrotum. These diagnostic techniques support the development of effective treatment plans by helping to determine the underlying cause of epididymitis.
Antibiotics are commonly used as a treatment for epididymitis, and they are usually given over one to two weeks. Rest, scrotal elevation, ice packs, proper hydration, and the use of nonsteroidal anti-inflammatory medicines (NSAIDs) to reduce pain are all examples of symptom management techniques. By reducing pain and inflammation, these two methods work together to aid in the healing process following epididymitis.
Complications from untreated epididymitis can include the development of an abscess, which is a pus-filled sac in the scrotum that may require surgical intervention or drainage. The scrotum's skin might also open due to severe oedema and inflammation. In rare cases, epididymitis can also worsen reproductive problems by interfering with sperm transport or production. It is crucial to seek medical assistance for epididymitis symptoms as early diagnosis and fast treatment dramatically lower the likelihood of severe problems.
By using condoms during safe intercourse, avoiding strenuous lifting, and taking breaks from extended sitting to increase blood circulation, people can lower their risk of developing epididymitis. By preventing groin injuries and STDs you can decrease the vulnerability to epididymitis, these interventions support urological health.
Home Dhakuria Specialities Andrology Epididymitis

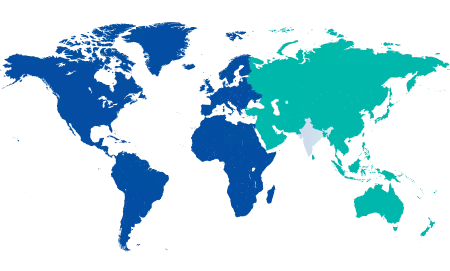
You’re on Our Indian Website
Visit the Global site for International patient services











