-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

ERCP Complicated Procedure
ERCP Complicated Procedure in Dhakuria, West Bengal
Endoscopic retrograde cholangiopancreatography (ERCP) is a combined endoscopic and fluoroscopic protocol in which an endoscope is advanced into the duodenum's second part, allowing other tools to be passed into the biliary and pancreatic ducts via the major duodenal papilla. Contrast material can be injected into these ducts to allow for radiologic visualisation and, if necessary, therapeutic intervention. ERCP began as a diagnostic complicated procedure treatment in Dhakuria involving cannulation of the pancreatic and biliary ducts but has since evolved into a therapeutic tool. This activity discusses the indications and techniques for endoscopic retrograde cholangiopancreatography, as well as the role of the interprofessional team in the management of patients undergoing this procedure.
Objectives
-
Determine when endoscopic retrograde cholangiopancreatography is indicated.
-
Describe the procedure for performing endoscopic retrograde cholangiopancreatography.
-
Describe the risks of endoscopic retrograde cholangiopancreatography.
-
Explain interprofessional team strategies for improving care coordination and communication, as well as promote the appropriate and effective use of endoscopic retrograde cholangiopancreatography.
Procedure
Endoscopy is used in ERCP to locate the major and minor papillae. Cannulation is performed, and contrast material is injected to identify the biliary and pancreatic ductal systems. Diagnostic procedures, such as cholangiopancreatoscopy, biopsy, or brush cytology, can be performed during ERCP. An intraductal ultrasound may be performed as well. Sphincterotomy, stent placement, and stone removal are all therapeutic applications.
Obstructive jaundice, biliary or pancreatic ductal system disease treatment or tissue sampling, suspicion of pancreatic Cancer, pancreatitis of unknown cause, sphincter of Oddi manometry, nasobiliary drainage, biliary stenting for strictures and leakage, drainage of pancreatic pseudocysts, and balloon dilation of the duodenal papilla and ductal strictures are all indication Sphincterotomy is used to treat sphincter of Oddi dysfunction or stenosis, difficulties with biliary stenting or accessing the pancreatic duct, biliary strictures, bile duct stones, bile sump syndrome after choledochoduodenostomy, choledochocele, and poor surgical candidates with ampullary carcinoma.
Implementation
Endoscopic papillectomy, sphincter of Oddi manometry, sphincterotomy, endoscopic papillary balloon dilation, stone removal, tissue sampling, placement of biliary and pancreatic stents, cholangiopancreatoscopy, and biliary and pancreatic drainage are all techniques used in ERCP.
The procedure begins with the duodenoscope being passed through a mouthguard. The duodenoscope is then advanced into the duodenal bulb via the stomach pylorus. A protuberance at the junction of the horizontal and vertical duodenal folds is inserted to visualise the major duodenal papilla, and the scope should be advanced to the second part of the duodenum. The major duodenal papilla is then cannulated. The recommended wire-guided technique involves inserting a guidewire into the common bile duct or pancreatic duct before injecting contrast.
Technicalities
The dual operator system, also known as the mother-baby system, requires two endoscopists to operate, with one endoscopist controlling the mother duodenoscope and the other endoscopist controlling the baby cholangiopancreatoscope, with a tip that is only deflectable in one plane, up and down.
The SpyGlass technique is catheter-based, with the optical probe passing through a 4-lumen catheter with a deflectable tip up-down and right-left. The cholangioscope is passed through the 1.2 mm working channel of the therapeutic duodenoscope, over a guidewire, into the biliary duct in both the dual and single operator techniques. Consult with the best doctors to learn more about ERCP Treatment in Dhakuria at Manipal Hospitals.
FAQ's
You may need an ERCP if you have any of the following symptoms, which could indicate a problem with your biliary system:
-
Sharp upper abdominal pain
-
Symptoms of jaundice, such as a blocked or leaking bile duct
-
Cholangitis, or inflammation of the bile duct
-
Scar tissue-induced narrowing (biliary stricture).
-
Gallstones in the bile duct
-
Pancreatitis due to gallstones
-
Cancerous tumours in your bile ducts
-
Injuries or leaks in the bile ducts
Endoscopy and fluoroscopy (a moving X-ray) are combined in ERCP. You can see how well fluids are moving through your biliary ducts with a fluoroscopy. Your provider will be able to detect any fluid leaks or stalling and backing up in your biliary system and investigate the cause of the problem.
An endoscopist can physically approach the spot with the use of the endoscope. This is how the contrast dye that is used in fluoroscopy is injected. It also enables them to address problems as soon as they arise. Endoscopists can pass long, narrow instruments through an endoscope for small procedures.
Conditions about your digestive system, which includes your biliary system, are the speciality of gastroenterologists. They are also experts in doing endoscopies. They receive training in endoscopic operations, which can serve as a stand-in for small surgeries.
Before your surgery, you will get personalised instructions from your healthcare professional. You may expect the following:
-
The healthcare provider will explain the procedure, and you may ask any questions.
-
They may ask for a consent form, which should be read carefully.
-
Patients with allergies to contrast dye, iodine, medicines, latex, tape, or anaesthesia should inform their healthcare provider.
-
A special diet may be advised for 1 to 2 days before the procedure.
-
Patients with bleeding disorders or blood-thinning medications should inform their healthcare provider.
-
Antibiotics may be prescribed for those with heart valve disease.
-
The procedure will involve anaesthesia, which may cause complete sleep or no sensation.
-
A sedative may be administered, and a driver will be needed.
-
Follow any other instructions given by the healthcare provider.
An ERCP can be performed as part of your hospital stay or as an outpatient procedure. The course of action may change depending on your health and the guidelines of your healthcare provider.
An ERCP typically goes through this procedure:
-
You will have an intravenous (IV) line inserted into your hand or arm.
-
During the surgery, you can receive oxygen through a tube in your nose.
-
On the X-ray table, you will be placed on your left side or, more frequently, on your stomach.
-
Your healthcare professional may spray numbing medication into the back of your throat.
-
An endoscope will be inserted through your mouth and then slowly moved down your stomach and oesophagus to the top of your small intestine (duodenum). Images are projected onto a screen.
-
Your provider will find the entrance to your duodenum's pancreatic and bile ducts with the help of projected images.
-
Once the endoscope catheter reaches this aperture, a smaller tube is inserted through it and slides inside. This is used with a tiny catheter to inject contrast dye into the ducts.
-
Your healthcare provider will take live video X-rays using fluoroscopy while the dye passes through the ducts. Fluoroscopy uses short bursts or pulses of X-ray rays to operate. It is regarded as a safe radiation exposure level.
-
At last, your doctor will examine these pictures for any issues with your ducts, such as leaks, enlargements, or clogs.
You'll need to stay in the medical facility for an hour or two after the surgery while the anaesthesia wears off. Your driver can then transport you home. After the treatment, you can experience mild discomfort for one or two days. Possible symptoms include:
-
Swallowing difficulties and a sore throat: It's possible that the endoscope inflamed your throat. Limiting your intake to soft meals or liquids until it feels normal again may be helpful.
-
Stomach discomfort or bloating: To improve visibility, the endoscope inflates your gastrointestinal system by blowing gas into it. The discomfort can pass once the gas is released through flatulence or burps.
-
Nausea: This could be an adverse effect of anaesthesia that goes away the next day.
The risks involved depend on the nature of the therapeutic procedure you undergo during ERCP as well as your pre-existing diseases. Any potential risks will be discussed in advance with you by your gastroenterologist.
Among the potential issues are:
-
Reaction to sedative agent: Cardiopulmonary problems may arise from anaesthetics in individuals who already have a heart or lung illness.
-
Allergic response to the colour used in contrast: Your doctor will promptly give you medication to stop the reaction if this occurs.
-
GI tract damage resulting from endoscopic procedures: This might result in internal bleeding or, in more serious situations, a hole.
-
A bile leak could result from endoscopic tools injuring your bile ducts.
-
Infection within the biliary tract: To avoid this, your doctor could prescribe antibiotics to you beforehand.
-
Pancreatic irritation.
Home Dhakuria Specialities Medical-gastro Ercp-complicated-procedure

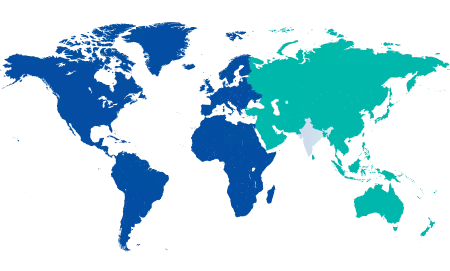
You’re on Our Indian Website
Visit the Global site for International patient services











