-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Cervical Biopsy
Best Cervical Cancer Treatment in Dhakuria, Kolkata
During a Cervical Biopsy, a small sample of tissue is taken from the cervix, and the cells are inspected under a microscope to look for any anomalies. Cervical Biopsies are performed to identify cervical cancer or precancerous cells. The endocervix and the exocervix are the two sections of the cervix. The higher portion that connects to the uterus is called the endocervix and the lower region that is exposed to the vaginal canal is called the exocervix. The "transformation zone," which is located between these two regions, is where cancer cells most frequently arise in the case of cervical cancer.
When a Pap smear produces abnormal results, clinicians perform a Cervical Biopsy, which includes taking a small sample of tissue to confirm or rule out malignancy. Being a candidate for this procedure does not guarantee that you have cervical cancer. Your physician or gynaecologist may also use a Cervical Biopsy to identify or treat certain problems, such as genital warts or polyps (noncancerous growths) on the cervix. Manipal Hospitals, the best Cervical Cancer Treatment in Dhakuria is backed by a team of professionals proficient in conducting such procedures with precision, thereby providing personalised treatment for your condition.
FAQ's
A Cervical Biopsy is a procedure where a small sample of cervix tissue is extracted and sent for further evaluation to the laboratory for examination under a microscope. The thin, lower end of the uterus that is situated at the end of the vagina is called the cervix.
Usually, a Cervical Biopsy is performed following the discovery of an anomaly during a standard pelvic exam or Pap screening. Atypicalities may encompass the existence of the human papillomavirus (HPV) or precancerous cells. Cervical cancer is the most prevalent cause of cancer globally, and certain kinds of HPV might increase your chances of getting it. Cervical cancer and precancerous cells can be detected with a Cervical Biopsy.
Finding malignant or precancerous cells in the cervical tissue requires a Cervical Biopsy. The following conditions may also need a Cervical Biopsy:
-
A positive test for high-risk strains of the human papillomavirus (HPV) or an abnormal Pap smear
-
Irregularities found during a pelvic check
-
Abnormal findings from imaging tests (ultrasound, magnetic resonance imaging, or computed tomography) that point to cervical cancer
-
Cervical cancer symptoms include vaginal bleeding during sex, heavy or irregular menstrual flow, pelvic discomfort, and vaginal discharge
-
Furthermore, vaginal warts or cervical polyps may occasionally be diagnosed with a Cervical Biopsy
-
A medical professional may also decide to do a Cervical Biopsy on a pregnant woman whose mother used diethylstilbestrol (DES). This drug is linked to causing reproductive cancers
There are three different types of Cervical Biopsies:
-
Punch Biopsy using a Colonoscopy: small parts of tissue using forceps are removed from the cervix using this technique. Your doctor may use a dye to stain your cervix to better see any irregularities.
-
Cone-based Biopsy: big, cone-shaped tissue fragments from the cervix are removed during this procedure using a knife or laser. A general anaesthetic will be administered to you, making you fall asleep.
-
ECC, or Endocervical Curettage: cells from the endocervical canal (the space between the uterus and vagina) are taken out during this surgery. A device carried in the hand called a "curette" is used for this.
-
If you have any allergies or sensitivities to latex or other drugs, inform your healthcare professional about this. It's also critical to let your doctor know about any drugs you take, as some may make bleeding more likely. Among these drugs are: Leve (naproxen), Aspirin, Advil (ibuprofen), and blood thinners such as Coumadin (warfarin).
-
If and when you should stop taking these drugs before your Cervical Biopsy will be determined by your healthcare practitioner.
-
For 24 hours before the procedure, avoid using douches, vaginal creams, medications, or tampons.
-
You should also avoid sexual activity for 24 hours prior to a Cervical Biopsy.
During a Cervical Biopsy, you can expect the following:
-
The consultation will start with a standard pelvic exam.
-
On an examination table, you will lie down.
-
Next, in order to numb the region, your doctor will administer a local anaesthetic.
-
You will be given a general anaesthetic to put you to sleep if you are having a Cone Biopsy.
-
The vaginal canal will then be kept open during the process by your doctor by inserting a speculum, a medical device, into the vagina. First, the cervix is cleaned using a vinegar and water solution.
-
While there may be some burning sensation involved, this cleansing procedure shouldn't hurt.
-
Iodine swabs can also be used to examine the cervix.
-
This examination, known as Schiller's test, aids your physician in determining whether any tissues are abnormal.
-
The surgeon will use a curette, a scalpel, or forceps to remove the abnormal tissues. If you are using forceps to remove the tissue, you can get a small pinching feeling.
-
To minimise bleeding after the Biopsy, your doctor could place absorbent material inside your cervix. This is not necessary for every Biopsy.
-
You may need to use a restroom once the speculum is withdrawn, and the medical professional or a nurse will provide you with towels to clean away any blood or discharge. A sanitary napkin could also be necessary if you're bleeding or have discharge.
-
Your recovery will vary depending on the kind of Biopsy you had and if you were sedated.
-
Once you're in the recovery area and no longer feel sleepy and your respiration, pulse, and blood pressure stabilise, you will be discharged from the hospital.
After a Cervical Biopsy, it's common to have slight cramps, spotting, and a dark or black discharge for a few days. As directed by your physician, use pain medication if necessary to ease cramps.
After a Cervical Biopsy, the majority of medical professionals advise not having intercourse or using tampons for up to two weeks. There may also be restrictions on some activities. Following a Cone Biopsy, recuperation time might take several weeks.
The risks associated with Cervical Biopsy depend on the type of Biopsy being done:
-
Colposcopic or Punch Biopsy: A solution used to reduce bleeding may cause a patient to have adverse effects such as dark-coloured vaginal discharge following the Biopsy. She could also bleed a little bit and have cramps or mild discomfort.
-
Cone Biopsy: These could include bleeding, infection, or scarring of the cervix. The patient may be more susceptible to premature delivery in the future if she has had a larger quantity of tissue removed, although having a Cone Biopsy does not always raise the chance of developing reproductive issues.
-
Cold Knife Excision: There might be additional risks associated with this kind of Biopsy, such as the possibility of a subsequent second-trimester miscarriage. If the patient has a Cone Biopsy and then gets pregnant, she has to make sure the medical team is aware of it. Menstrual periods may hurt more as a result of the cervical scarring. If the patient gets pregnant after this treatment, there is also a chance that the baby will be born early.
Home Dhakuria Specialities Obstetrics-and-gynaecology Cervical-biopsy

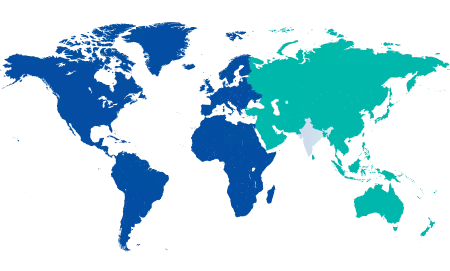
You’re on Our Indian Website
Visit the Global site for International patient services
Your Feedback is Highly Valued!












