-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Menopause Clinic
Menopause Clinic in Dhakuria, West Bengal
Menopause is a significant phase in a woman's life that can bring various challenges. While it is a natural process, some women may experience severe symptoms that require medical attention. Our Menopause Clinic at Manipal Hospitals in Dhakuria, West Bengal, is dedicated to providing comprehensive care to women undergoing this transition.
Some of the conditions and symptoms managed at our Menopause Clinic include:
-
Severe hot flashes
-
Night sweats
-
Vaginal dryness and discomfort
-
Osteoporosis and bone health concerns
-
Mood swings and depression
-
Sleep disturbances
-
Hormonal imbalances
Research indicates that not addressing these symptoms can significantly impact a woman's quality of life. However, treatments and interventions, when carefully managed, can alleviate these symptoms and improve overall well-being. Our team of expert gynaecologists at Manipal Hospitals frequently monitors the health of women experiencing menopause and recommends appropriate treatments tailored to individual needs. Manipal Hospitals provides the best Menopause Treatment In Dhakuria.
FAQ's
The doctor will review your medical history, including current medications, previous surgeries, and family history. We will attentively listen to your experience to create a tailored and comprehensive treatment plan to help you manage your symptoms and enhance your quality of life. This plan may include prescription HRT (Hormone Replacement Therapy), other medications as needed, and lifestyle recommendations.
It is customised based on personal health risks and advantages. The advice is intended to relieve symptoms and promote long-term health. This includes symptomatic women with complex or high-risk illnesses such as breast cancer, familial breast cancer, cardiovascular disease, or osteoporosis.
Menopause usually happens between ages 45 and 55 and marks the end of a woman's ability to have children, which is a natural part of getting older. Menstrual cycles end as women age because their ovaries produce less progesterone and oestrogen. Surgical procedures, such as the removal of the ovaries or a Hysterectomy, can also trigger menopause. Medical treatments like Chemotherapy and Radiation can damage the ovaries and cause early menopause. Additionally, certain health conditions like autoimmune disorders or a family history of early menopause can influence the timing.
Yes, during menopause, periods can stop suddenly. This occurs because the ovaries gradually produce less oestrogen and progesterone as a woman ages. As hormone levels fluctuate and eventually decline, menstrual cycles may become irregular and eventually stop altogether. This transition typically occurs over a period of time, but for some women, periods can cease abruptly.
The menopausal transition, or perimenopause, refers to the years preceding menopause when women may experience changes in their monthly cycles, hot flashes, or other symptoms. The transition to menopause typically starts between the ages of 45 and 55.
Changes in menstruation patterns and the advent of hot flashes are frequently the first indications. Although blood tests are not required, healthcare practitioners can use blood or urine samples to assess levels of oestradiol, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).
Postmenopause is the phase after menopause when a woman has not had a period in over a year. Although you will no longer have periods after menopause, some women may still have menopausal symptoms such as hot flashes, night sweats, vaginal dryness, mood changes, and sleep disturbances.
Oestrogen is the main hormone in menopause. Before menopause, the ovaries slowly produce fewer mature eggs, and ovulation becomes irregular. During this time, there's also a decrease in oestrogen and progesterone production. Oestrogen is important for controlling the menstrual cycle and keeping reproductive health in balance.
A woman who gets a Hysterectomy but preserves her ovaries does not experience menopause immediately. Because your uterus has been removed, you no longer have periods and cannot become pregnant. However, your ovaries may still produce hormones, so you may not experience other symptoms of menopause. Later on, you can experience natural menopause a year or two earlier than intended. A lady who has both ovaries removed simultaneously with her Hysterectomy goes into menopause right away. Bilateral Oophorectomy refers to the removal of both ovaries. Women who undergo this operation no longer have periods and may experience menopausal symptoms right away.
Yes, menopause can result in bone loss. During menopause, oestrogen—a hormone that supports bone density—decreases dramatically. This hormonal change can lead to accelerated bone loss, increasing the risk of osteoporosis and fractures. Bone loss can weaken bones, making them more likely to break. Osteoporosis occurs when bones deteriorate significantly. Weight-bearing physical activity, such as climbing stairs, walking, or lifting weights, is necessary for women to maintain strong bones. You can also safeguard your bone health by consuming calcium- and vitamin D-rich foods or by taking vitamin D and calcium supplements as needed. Not smoking also protects your bones.
Yes. Women who have gone through menopause are more likely to experience cardiovascular disorders such as heart attacks and strokes. Changes in oestrogen levels may be a contributing factor. This is because, as you age, you may gain weight and acquire other health issues that raise your risk of cardiovascular disease. Consult your doctor about critical tests such as cholesterol and elevated blood pressure.
For females with uteruses, HT consists of the hormones oestrogen and progesterone. Women who no longer have a uterus use oestrogen alone. Most of the oestrogen prescription is bioidentical oestradiol, administered through the skin for increased safety. HT can be extremely effective at relieving moderate-to-severe menopausal symptoms and avoiding hip fractures. However, HT is not for everyone.
A specialist will conduct an individual risk assessment and advise you on how to lower your risk of blood clots, heart attacks, strokes, breast cancer, and gallbladder illness, all of which are connected with HT.
Avoid using HT if:
-
You think you are pregnant.
-
Have undiagnosed vaginal bleeding
-
Have had breast or uterine cancer
-
Have suffered a stroke, heart attack, or blood clots
Home Dhakuria Specialities Obstetrics-and-gynaecology Menopause-clinic

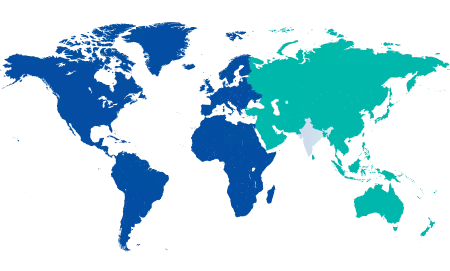
You’re on Our Indian Website
Visit the Global site for International patient services











