-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Complexities in Oesophagectomy Gastrectomy and Colectomies
Complexities in Oesophagectomy, Gastrectomy and Colectomies in Dhakuria, West Bengal
The procedure known as an Oesophagectomy is the removal of all or part of your oesophagus, which is the tube that carries food from your neck to your stomach. This operation is typically carried out by surgeons to treat oesophagal cancer. This is a major surgery where the diseased tissue is removed. Your digestive tract is then rebuilt so that you can eat normally.
A Gastrectomy is a surgery to remove the stomach. During a Total Gastrectomy, your entire stomach is removed. Your stomach is removed in part during a Partial Gastrectomy. This procedure is used to treat extreme obesity, stomach cancer, or other stomach diseases that don't improve with non-surgical methods like medicine and lifestyle modifications.
Removal of the colon is called a Colectomy. At the end of your digestive tract lies a long, tube-like organ called your colon, which is a portion of your large intestine. To cure or prevent illnesses and disorders that affect your colon, a Colectomy could be required.
There is an increased risk of developing infections or complications following an Oesophagectomy, a Gastrectomy, or a Colectomy. Patients must receive comfortable care during this delicate state of recovery with appropriate infection control measures. Manipal Hospitals is the best hospital for surgeries for complexities In Oesophagectomy Gastrectomy And Colectomies.
FAQ's
A person may require an Oesophagectomy in the following cases:
-
Oesophageal cancer
-
Conditions like Barrett’s oesophagus (a change in the structure of the oesophagus) increase the risk of oesophagal cancer
-
Non-cancerous conditions of the oesophagus
You will be given anaesthesia before surgery to make you unconscious and ensure a painless procedure. Your surgeon will make one or more incisions in your neck, chest, or belly, depending on the surgery, to get access to your oesophagus. Your oesophagal portion that is affected will be removed by your surgeon. In some cases, a small portion of the stomach may be removed. In extreme circumstances, your entire stomach could have to be removed.
Depending on the kind of surgery, the surgeon will draw your stomach (or small intestine) up into your chest or neck region and reattach it to the remaining oesophagus.
Your surgeon will remove your lymph nodes to test them in a lab for cancer cells if you have oesophagal cancer. The presence of cancer cells in your lymph nodes indicates that the disease has progressed beyond your oesophagus.
Whatever kind of Oesophagectomy you have, you will require a feeding tube to get nutrients while your swallowing capacity heals. The tube will be inserted into your small intestine or stomach by your surgeon. In addition, a nasogastric tube—a drain that enters via your nose—will be attached to you. This tube aids in healing by sucking out extra air from your stomach. To release fluid that builds up in your chest cavity, you could also require chest drains. This aids in healing as well.
After surgery, adverse consequences are frequently seen. Your medical team will keep an eye on your well-being and assist with symptom management. Among the side effects are:
-
Decreased appetite
-
Discomfort when swallowing
-
Gas, bloating, and heartburn
-
Vomiting and nausea
-
Respiratory issues, the most prevalent of which is pneumonia
-
Leaking at the anastomotic point, which is the junction of your stomach and oesophagus
-
Atrial fibrillation (an irregular heartbeat that can reduce blood flow)
-
Dysphagia (inability to swallow or talk)
-
Bleeding and infection at the surgical site
-
Acid reflux
As you recover, most of these symptoms usually go away, but others (like digestive issues) cannot.
A Gastrectomy is required in the following conditions:
-
Non-cancerous stomach growths: removal may be necessary for tumours that exhibit symptoms or have the potential to progress to malignancy.
-
Infection in the stomach: rarely, stomach lining inflammation can result in severe symptoms that cannot be treated by medicine. Surgery could be necessary in such cases.
-
Peptic ulcers: to heal stomach sores and ulcers that might harm the stomach lining, surgery can be necessary.
-
Obesity: a doctor could suggest a Partial Gastrectomy as a kind of bariatric (weight loss) surgery.
-
Accidents: if an injury has affected your stomach's tissue beyond repair, you could need to have some of it removed.
Anaesthesia is administered to put the patient to sleep during the operation. During surgery, a surgeon removes parts of the stomach employing an Open surgery, or laparoscopy technique. Lymphadenectomy may be performed to detect the spread of cancer. The surgeon then reconstructs the digestive system by attaching the remaining organs, such as the small intestine, to the stomach or oesophagus. A feeding tube may be inserted to aid recovery. The cut is then stitched to ensure proper healing. Catheters may be placed to collect urine, and a nasogastric tube may be used to suction stomach contents.
The following are potential Gastrectomy side effects:
-
Food moves too rapidly from your stomach into your bowel (dumping syndrome)
-
Acid reflux
-
Diarrhoea
-
Chest disorders such as pneumonia and bronchitis
-
Internal haemorrhage
-
Vomiting and nausea
-
Stomach acid seeps into your oesophagus, resulting in constriction and scarring
-
Vitamin deficiencies
-
Unintentional loss of weight
Colectomy is used to treat and avoid the following disorders and diseases that affect the colon:
-
Bleeding: surgery may be necessary to remove the colonic section that is bleeding excessively.
-
Blockage of the bowel: in an emergency, a clogged colon may necessitate a whole or Partial Colectomy, depending on the circumstances.
-
Colon cancer: Colectomy may only need to remove a tiny portion of the colon in cases of early-stage malignancy. Later-stage cancers can require removing more colon tissue.
-
Crohn's disease: an inflammatory disorder of the colon that causes swelling of the tissues of the digestive system. Removing the affected portion of your colon may provide short-term relief from symptoms if medicine isn't working for you.
-
Ulcerative colitis: inflammation and ulcers in the digestive tract.
-
Diverticulitis: inflammation of the diverticulum (pockets inside the colon).
-
Preventive surgery: if someone is at a high risk of colon cancer due to the formation of multiple precancerous colon polyps, they may need to undergo a Total Colectomy to prevent cancer in the future.
During the procedure, general anaesthesia will be given to you. These medications put you to sleep, so you won't experience pain during surgery. Your medical team will hook you up to monitors so they can keep an eye on your blood pressure, heart rate, and respiration. Your belly's skin will be cleansed, and any hair in that area may be shaved or trimmed.
Your stomach will have a long incision made by the surgeon during an Open Colectomy. A Laparoscopic-assisted Colectomy will require many tiny incisions. The affected portion of your colon will be removed by the surgeon, and the exposed colon ends may be sewn together by the surgeon. Alternately, a stoma—an opening to the exterior of your body—will be created. The surgeon could remove lymph nodes close to the malignancy. The surgeon will seal the wound after the procedure.
Some common risks of a Colectomy are:
-
Reactions from anaesthesia
-
Pneumonia
-
Blood clots in the legs or lungs
-
Internal bleeding
-
Infection at the incision site
-
Scarring in the stomach, which can lead to blockage of the intestines
-
Leaking, where the intestines are sewn together
-
Damage to adjacent organs
Home Dhakuria Specialities Organ-transplant Complexities-in-oesophagectomy-gastrectomy-and-colectomies

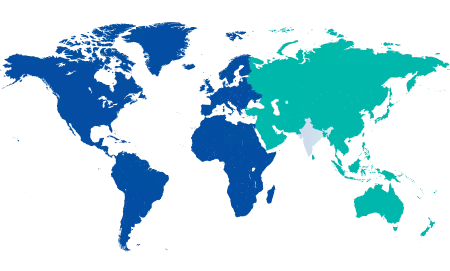
You’re on Our Indian Website
Visit the Global site for International patient services











