-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Oesophagectomy Gastrectomy and Colectomies
Oesophagectomy, Gastrectomy, and Colectomies in Dhakuria, West Bengal
Oesophagectomy
The Oesphagectomy procedure involves the removal of the partial or whole oesophagus present between the mouth and the stomach and reconstructing or joining together the remaining parts of the oesophagus and stomach. The procedure is usually done to address early or advanced stages of oesophageal cancer, Barrett’s oesophagus, and other conditions like oesophageal strictures or achalasia.
Gastrectomy
The Gastrectomy procedure involves the removal of the stomach. The procedure is usually done to treat bleeding and inflammation, early and advanced stages of gastric cancer, and polyps or growth that are present on the lining of the stomach.
Colectomy
The Colectomy procedure involves removing the colon or large intestine. The procedure is typically employed to address and treat individuals diagnosed with early and advanced stages of colon cancer and severe cases of inflammatory bowel disease (IBD). In colon cancer, the procedure is done based on the stage of the cancer and the location of the tumour.
At Manipal Hospitals, Dhakuria, West Bengal, the Department of Organ Transplant is adept at handling various surgical interventions mentioned above with precision and accuracy, with the help of cutting-edge modalities and treatment methodologies housed at the institution. Manipal Hospitals is the best place for Oesophagectomy Gastrectomy And Colectomies.
FAQ's
Whether you require an Oesophagectomy, Gastrectomy, or Colectomy, the usual process includes evaluating your symptoms and a physical evaluation. This is followed by a thorough screening and diagnostic imaging assessment, such as blood tests, endoscopic diagnostic interventions, computed tomography (CT) scans, and magnetic resonance imaging (MRI) scans. Based on the examination, our specialists will discuss with you appropriate treatment interventions to address your condition, its possible risks or complications, medications, and post-procedural care.
Specialists employ several diagnostic interventions, including lab tests and imaging scans, which include, but are not limited to, blood sugar and blood pressure levels, endoscopic ultrasound-guided fine needle Biopsy, urinalysis, Colonoscopy, CT, MRI, or positron emission tomography (PET) scans. Biopsy procedures are done for all three procedures to confirm the presence of cancer as well as to determine the grade and stage of the disease. Sometimes, molecular tests will be done, such as confirming the mutation of the CDH1 gene that verifies hereditary gastric cancer. Individuals with the CDH1 mutation are generally recommended to undergo Total Gastrectomy.
Our specialists will give you personalised instructions regarding preparing for surgery. However, general guidelines and instructions include the following:
-
In oesophageal cancer, depending on the size of the tumour, our specialists may recommend undergoing Chemotherapy or Radiation Therapy to shrink the tumour to a considerable size prior to surgery.
-
You will have to inform your specialist if you are taking medications like anti-coagulants, SGLT2 inhibitors, prescription medicines, over-the-counter medicines, or any implanted medical devices, such as pacemakers.
-
If you are a smoker, refrain from smoking at least 2 weeks prior to surgery, as it could manifest in surgical complications.
-
Consumption of alcohol can lead to serious complications. Therefore, it is crucial to inform your specialist to avoid any severe post-withdrawal symptoms and risks.
-
Manage your blood sugar, cholesterol, and blood pressure levels to reduce any risks.
-
It is necessary to discuss with our specialists the duration of your stay at the hospital and plan your must-haves and comfort items accordingly.
Yes, Oesophagectomy, Gastrectomy, and Colectomy are major procedures that are done based on the severity of your condition and individual factors. Although performed as an open surgery, advancements have been made in performing all the procedures with minimally invasive techniques using Laparoscopy methods and Robotic-assisted Surgery. However, the type of invasiveness required depends on parameters like the location and depth of the tumour, the patient’s overall health, past surgeries, and existing commodities.
Recovery time for these surgeries varies depending on the type of surgery and the patient’s overall health. Generally, some patients spend several days to weeks in the hospital, while others take less time. To enhance recovery time, it's important to follow all post-operative care instructions, such as taking medications for pain management, gradually reintroducing eating and drinking, and monitoring for complications. Full recovery can take several weeks to months, and patients may need to adjust their diet and lifestyle permanently.
There are several benefits offered to patients undergoing minimally invasive Oesphagectomy, Gastrectomy, and Colectomy in contrast to Open-surgery, which include:
-
Faster recovery
-
Less pain
-
Few incisions with minimal depth
-
Less duration of hospital stays
-
Reduced bleeding
-
Fewer complications
-
Reduced scarring
Risks or complications associated with these procedures often stem from inexperienced surgeons performing the surgery. Specialists at Manipal Hospitals, Dhakuria, West Bengal, are equipped with the skills to perform Minimally Invasive and Robotic-assisted procedures to achieve optimal patient outcomes.
You will have to seek immediate attention if you notice the following post-operative symptoms:
-
In Oesophagectomy, vomiting blood, inability to swallow or breathe, high fever or chills, fatigue, heart palpitations, diarrhoea or black stools, a burning feeling in the throat, persistent cough, unexplained weight gain, and severe chest pain.
-
In Gastrectomy, nausea or vomiting, soft or bloody stools, diarrhoea, pain or pressure in the abdominal area, bloating, or any swelling, redness, or discharge like pus around the incision site.
-
In Colectomy, fever, shortness of breath, persistent cough, chest pain, irregular cardiac rhythm, discharge, infections or abnormal bleeding around the incision site, trouble urinating, uncontrolled bowel movements, and swelling for prolonged periods.
Home Dhakuria Specialities Organ-transplant Oesophagectomy-gastrectomy-and-colectomies

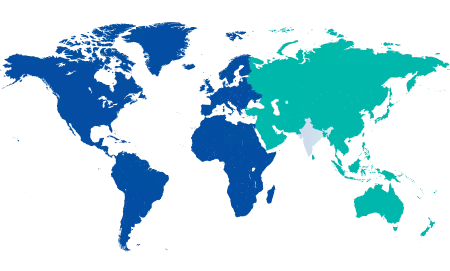
You’re on Our Indian Website
Visit the Global site for International patient services
Your Feedback is Highly Valued!












