-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Paediatric Haemato-oncology
Paediatric Haemato-oncology in Dhakuria
Paediatric Haemato Oncology is a speciality that provides comprehensive oncology services for blood disorders and cancers in children under the age of 18. In this field, healthcare providers treat some of the most critically ill and challenging cases of leukaemia, sickle cell anaemia, lymphoma, and various types of anaemia. The dedicated team of specialists in paediatric oncology and haematology consists of haematologists, paediatric oncologists, radiation oncologists, paediatric oncology residents, nurses, child psychologists, and social workers. They work tirelessly and in collaboration to ensure that every child receives the highest quality treatment for their condition.
It is essential to discover signs of blood cancer as soon as possible through screening tests and careful observation. Manipal Hospitals, Dhakuria, has a team of experienced paediatric haemato-oncologists who employ advanced diagnostic techniques and treatment approaches tailored to each child’s unique needs. In addition to medical treatment, these specialists provide comprehensive care that encompasses psychological support, pain management, and nutritional guidance to ensure the child's and their family's overall well-being. The goal is not only to treat the disease but also to support the child’s growth, development, and quality of life during and after treatment.
FAQ's
Some of the most prevalent conditions treated in this division are:
-
Leukaemia: This condition affects the bone marrow and blood and includes acute lymphoblastic leukaemia (ALL) and acute myeloid leukaemia (AML).
-
Lymphoma: Conditions affecting the lymphatic system, including non-Hodgkin and Hodgkin lymphomas.
-
Neuroblastoma: A cancerous growth that develops from undeveloped nerve cells, often found in the nerves surrounding the spinal cord or in the adrenal glands, affecting infants and young children.
-
Wilms tumour: Kidney cancer of this kind usually affects young patients.
-
Thalassemia: A genetic blood disorder in which the body makes an abnormal form of haemoglobin.
-
Myelodysplastic syndromes (MDS): These are a group of disorders caused by dysfunctional or poorly formed blood cells.
These conditions require specialised care that combines medical treatment, supportive care, and psychosocial support to manage the complex needs of paediatric patients.
If your child experiences any of these symptoms, seek a visit to a paediatric haemato-oncologist or refer your child’s physician for an accurate diagnosis. These symptoms are not typically of blood disorders or cancer but also of other illnesses.
-
Unexplained bleeding or bruises that are difficult to manage
-
Unexplained high body temperatures
-
Joint or bone pains, occasionally coupled with oedema
-
Recurrent diseases or infections
-
Fatigue or pallor, despite getting enough sleep
-
Inflamed lymph nodes under the arms, groyne, or neck
-
Pain or swelling in the abdomen
-
Headaches, convulsions, or vision abnormalities (for disorders relating to the brain)
-
Breathing problems or shortness of breath
-
Anaemia-related symptoms such as weakness, dizziness, or dyspnea
Paediatric oncologists perform specific tests to detect the presence of blood cancers. These results aid in the identification of the type and risk level of blood cancers, which are directly linked to the prognosis or severity of the disease.
-
PET scan: A PET scanner uses a mildly radioactive substance to identify regions of your body with heightened cellular activity, providing insights on potential cancer spread.
-
A complete blood count (CBC): It is a type of blood test that is used to assess one's overall well-being. It can identify various blood-related illnesses and types of cancer.
-
CSF analysis: Under anaesthesia, CSF examination via lumbar puncture looks for leukaemia cells in the cerebrospinal fluid to identify the possible spread of acute lymphoblastic leukaemia (ALL).
-
Chromosomal analysis: To accurately diagnose leukaemia, bone marrow cells are subjected to chromosomal analysis, or karyotyping, which looks for genetic abnormalities in leukaemia cells.
The initial phase of treatment typically involves addressing the initial signs, which often consist of bleeding, infection, and/or anaemia (insufficient red blood cells).
-
Chemotherapy: Destroys cancer cells or inhibits their proliferation with medication
-
Radiation Therapy: Targets and kills cancer cells with high-energy radiation
-
Surgery: Removes malignant tissue or tumours from the body
-
Immunotherapy: Increases immunity to combat cancerous cells
-
Targeted Therapy: A medication-based approach to target particular genetic alterations in cancer cells
-
Stem Cell Transplantation: Uses healthy stem cells to replace damaged bone marrow
-
Supportive Care: Enhances quality of life by managing symptoms and adverse effects
In paediatric Haemato-oncology, early identification is essential to enhancing treatment results and survival rates. It makes rapid and efficient interventions possible, frequently with less drastic measures. Monitoring symptoms and getting regular checkups are crucial. The sooner children are diagnosed and treated, the better their chances are of living longer without any health complications. This is because early diagnosis not only improves their overall outlook but also allows for more effective treatments, even if a relapse occurs.
Many childhood blood cancers can be cured, especially with prompt and efficient treatment. Due to advancements in medicine, conditions like lymphoma and leukaemia are now more likely to be successfully treated. For affected children, early detection and personalised treatment greatly improve their chances of a successful outcome and long-term survival.
-
Adhere according to the paediatric oncologist's recommended treatment plan
-
Make sure the child follows the prescribed dosage and timing for taking their medications
-
Offer wholesome food to improve the child's general health and immune system
-
Promote regular exercise within the boundaries that the medical staff has advised
-
Reduce the risk of infections by keeping your home clean and hygienic
-
Keep a close eye on the child's symptoms and notify the healthcare professional right away if anything changes or causes worry
-
While keeping lines of communication open regarding the child's condition, provide emotional support and reassurance
Home Dhakuria Specialities Paediatric-and-child-care Paediatric-haemato-oncology

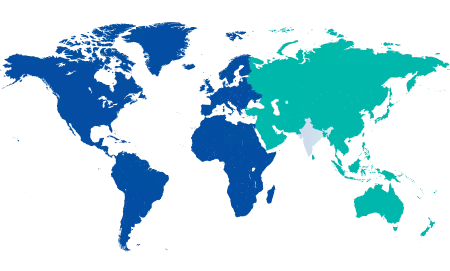
You’re on Our Indian Website
Visit the Global site for International patient services











