-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Dressing
Best Dressing and Wound Care in Dhakuria
In Plastic and Cosmetic Surgery, dressing plays an important part in the healing process after surgery. Following surgery, dressings offer a moist environment that promotes healing, absorbs exudates, and shields wounds from infection. Additionally, they aid in keeping the surgical site shaped, especially after Rhinoplasty or Abdominoplasty, by providing compression to lessen swelling and aid in the skin's adhesion to the underlying tissues. Depending on the particular requirements of the wound and surgical site, a range of materials, including silicone gels, hydrocolloids, and foam dressings, are used in modern dressings. For example, silicone dressings are frequently employed because of their capacity to lessen the appearance of scars and enhance their appearance. Another kind of dressing that is commonly used post-operatively to support tissues, lessen fluid collection, and improve contouring outcomes is compression garments. These dressings are essential for both promoting the best possible aesthetic outcome from the surgery and for the physical healing process. Careful selection and supervision by medical professionals are necessary to guarantee the patient's best possible recovery and the desired cosmetic result. For the best dressing and wound care in Dhakuria, you can visit Manipal Hosptals.
FAQ's
In the postoperative care of Plastic and Cosmetic Surgery, dressings have three functions: they absorb fluids, prevent infection, and keep the healing environment moist. They offer compression to support tissue, lessen oedema, and promote healthy skin adherence. Furthermore, dressings help to keep the surgical site in its original form, protect sensitive areas from pain, prevent scarring by using specialised materials, and make it easy to monitor for complications—all of which contribute to the best possible healing and cosmetic results.
Sealing the wound, preventing infection, and stimulating tissue regeneration are just a few of the ways silicone gels and hydrocolloids greatly facilitate the healing process. Silicone gels are excellent for pain relief, hydration, and scar management. In addition to providing thermal insulation and a wet environment, hydrocolloids also aid in autolytic debridement. Both dressings aid in the development of granulation tissue, epithelialization, and the management of inflammation. Hydrocolloids work well for pressure ulcers, burns, venous ulcers, and diabetic ulcers; silicone gels work well for scars and burns.
When choosing a dressing for surgical wounds, one must consider the location, size, depth, kind of wound, and exudate level. Selection is also influenced by the patient's characteristics, such as pain and allergies, healing status, and infection risk. Adhesion, flexibility, and ease of application are essential for dressings, particularly for areas that move. Cost, accessibility, and particular surgical requirements—like maintaining cleanliness and moisture levels are essential for promoting the best possible healing, preventing infections, and ensuring patient comfort.
Compression garments strengthen tissues, improve circulation, and lessen bruising and swelling during Plastic and Cosmetic Surgery. Through constant pressure, they help prevent seromas, lessen pain, and enhance scar formation. They also help with skin retraction, which guarantees a smooth, natural appearance after surgery. Compression garments are essential in the postoperative treatment of patients because of these advantages, which promote optimal healing, reduce problems, and support the intended surgical outcomes.
Complications, including infections, delayed healing, skin maceration, and allergic responses, can result from improper use or selection of post-surgical dressings. In addition, they can result in worsening discomfort, pressure sores, dehiscence of the wound (wound separation), excessive scarring, seroma formation (fluid buildup), and a delay in the detection of consequences. To preserve ideal moisture levels, shield the wound, and guarantee a quick and efficient healing process, the right dressing selection and application are crucial.
Following Plastic or Cosmetic Surgery, the frequency of dressing changes varies depending on the procedure, the state of the wound, and the surgeon's instructions. Depending on the exudate and dressing type, changes usually happen every 1-3 days after the initial 24-48 hour change. If difficulties, such as bleeding or infection, occur, quick adjustments are required. Always adhere to the precise instructions given by the surgeon, schedule regular follow-ups, and follow up as needed to maintain maximum healing.
Contemporary dressings regulate moisture, lower the risk of infection, and increase compliance and comfort to improve the aesthetic results following Plastic or Cosmetic Surgery. Silicone-based dressings help with scar care, while speciality products offer superior support and contouring. Their mild adhesion minimises healing interruption, and their personalisation and adaptability enable customised wound treatment. In comparison to conventional techniques, contemporary dressings generally encourage optimal wound healing, fewer complications, and better cosmetic outcomes.
Through compression, absorption, and fluid redistribution, dressings control post-surgery swelling and fluid accumulation. Compression clothing and bandages encourage the body to absorb fluid again, which lowers oedema. Certain absorbent dressings, such as hydrocolloids, disperse fluid away from the site, whereas others absorb excess exudate. Certain dressings promote a quicker recovery and fewer difficulties by facilitating lymphatic drainage, acting as barriers against pollutants, and maintaining the ideal moisture balance.
Healthcare practitioners monitor wound progress, apply dressings correctly, and make adjustments as necessary. They keep in touch to enable coordinated care, educate patients on dressing maintenance, and offer support. Precise record-keeping of modifications and evaluations monitors advancement and promotes care continuity. In the end, their supervision and management of surgical dressings support the best possible wound healing and the welfare of patients throughout their recuperation.

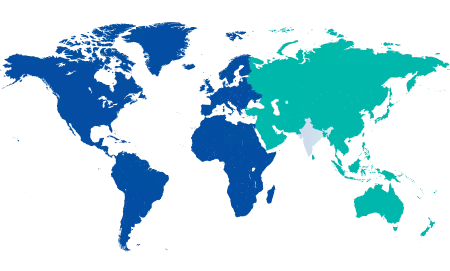
You’re on Our Indian Website
Visit the Global site for International patient services











