-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Minimally Invasive Spinal Stabilization
Minimally Invasive Spinal Stabilization in Dhakuria
Spine surgery can also be carried out with minimally invasive techniques. Minimally Invasive Spinal Stabilisation surgery aims to stabilise the spine with less disruption to the surrounding muscles and tissues compared to traditional open surgery. This technique involves making one or more tiny incisions through which specialised instruments and imaging guidance are used to place implants like screws, rods, or cages to stabilise the spine. The primary benefits of this approach include reduced blood loss, shorter hospital stays, less postoperative pain, and faster recovery times. Minimally Invasive Spinal Stabilisation is often used to treat conditions like spinal instability, degenerative disc disease, and spinal deformities, offering patients a quicker return to normal activities while minimising the risks associated with more invasive procedures.
At Manipal Hospitals, Dhakuria, the team of spine surgeons is highly experienced and employs advanced techniques to enhance patient outcomes, improving their quality of life.
FAQ's
Minimally invasive Spine Stabilisation surgery can be employed to address the following subsequent conditions:
- Spinal instability
- Spinal stenosis
- Trauma from a vehicle accident or athletic injury
- Injuries brought on by a fall from a height that include fractures and spinal compression
- Degenerative disc diseases such as herniated discs
- Spinal deformities like scoliosis or kyphosis
- Fractures in the spine caused by osteoporosis-related bone loss
Discuss surgical preparations with your healthcare practitioner, as you may be required to follow certain specific guidelines based on your condition. Tell your doctor about every prescription drug you are consuming, including aspirin and other over-the-counter medications. Certain medications, including blood thinners, may need to be discontinued before the surgery. You must give up smoking and other nicotine-containing products before your procedure, as nicotine may cause a delay in recovery. Consult your physician if you want assistance in quitting smoking. In addition, imaging examinations may be required prior to surgery. These might include MRIs or X-rays. Follow any instructions you receive on not eating or drinking anything prior to your procedure. Any recent changes in your health, such as a fever, should be reported to your healthcare professional beforehand.
A MISS will be done in the following steps:
-
You'll be given anaesthesia to numb your body parts. During surgery, this will help you to be awake yet comfortable. Or perhaps you will be put under general anaesthesia, making you sleep through the procedure and avoid pain as a result.
-
Throughout the procedure, your blood pressure and heart rate will be closely monitored by a medical professional.
-
Before and after the procedure, you can be prescribed antibiotics. This will help reduce the chances of an infection post-surgery.
-
Throughout the process, a specialised kind of X-ray will be used by your surgeon to see the surgery progress.
-
Your back will be slightly incised in the treated region by the medical professional. In this incision, a tubular retractor is inserted. This will make the affected area of the spine visible.
-
Next, the surgeon will insert tiny instruments via this retractor. This has a light and a little camera on it.
-
After that, your healthcare expert will fix the spine as necessary.
-
The tools and retractor are taken out once the repairs are completed. Stitches, glue, or staples are used to seal the wound or incisions. A small bandage is then applied to the wound.
After Minimally Invasive Spinal Stabilisation surgery, patients are typically monitored in the recovery room until the effects of anaesthesia wear off. You may experience some discomfort, swelling, or soreness at the incision site, which is normal and can be managed with pain medication prescribed by your doctor. Patients are encouraged to move gently and begin walking as soon as possible to promote circulation and reduce the risk of complications.
A physical therapist may assist with early mobility exercises and guide you on safe movements to avoid strain on the spine. Depending on the extent of the surgery and your overall health, you might be discharged the same day or within a few days.
Your doctor will provide specific post-operative instructions, including activity restrictions, wound care, and follow-up appointments to monitor your recovery. It's important to avoid heavy lifting, twisting, or strenuous activities during the initial healing period. Adhering to your rehabilitation plan and attending follow-up visits will help ensure a smooth recovery and the best possible outcome.
Recovery time will vary among individuals, but patients often experience a quicker recovery compared to traditional surgery, with many able to return to light activities within a few weeks. While the bones fuse together, limited activity is permitted; lifting, bending, and twisting should be avoided. Walking and stretching will be the initial exercises in physical therapy during the first week following surgery, and for the next two months, static stabilisation exercises will be the focus.
The advantages of Minimally Invasive Spinal Stabilisation surgery are as follows:
-
Smaller cuts
-
Reduction in surgical complications and blood loss
-
Less harm to the soft tissues and muscles around
-
Reduced chance of infection
-
Reduced need for powerful painkillers during recovery and decreased postoperative discomfort
-
Quicker recovery
-
Improved aesthetic outcomes with less scarring
While many patients are good candidates for minimally invasive techniques, the suitability depends on the specific condition, overall health, and the complexity of the spinal issue. Your surgeon will determine the best approach based on your individual case.
Home Dhakuria Specialities Spine-care Minimally-invasive-spinal-stabilization

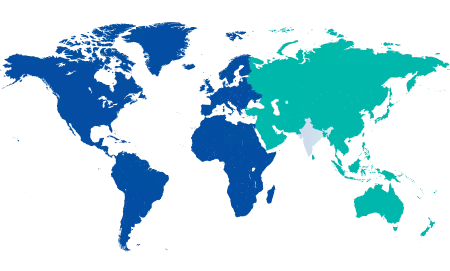
You’re on Our Indian Website
Visit the Global site for International patient services











