-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Postero Lateral Spinal Fusion PLF
Postero Lateral spinal fusion PLF in Dhakuria
The goal of Spinal Fusion Surgery is to stabilise the spine by decompressing the affected nerve and using bone grafts from the patient to permanently fuse vertebrae. It works by stopping the vertebrae from moving excessively, which effectively lowers pain. The type of Spinal Fusion Surgery that requires reaching the spine through the back is called Posterolateral Lumbar Fusion.
Although spinal fusion can greatly reduce pain, there are hazards associated with surgery, including the possibility of infection, blood clots, nerve injury, nonunion, or the failure of the bones to fuse properly. Physical therapy and activity restrictions are part of recovery to ensure appropriate healing and rehabilitation. While evaluating a patient's appropriateness for spinal fusion, medical professionals carefully evaluate all available options as well as the long-term effects on the patient's quality of life.
FAQ's
Posterior Lumbar Spinal Fusion helps alleviate pain and instability in the spine. Some common indications for the surgery are:
-
Degenerative Disc Disease: A condition where the disc between the vertebrae wears down, causing pain and instability in the spine
-
Spinal Fracture: Any fracture that develops in the spinal column can give rise to severe pain and instability
-
Scoliosis: A condition where the spine curves to one side. It exerts uneven pressure on the vertebrae, resulting in pain and often requiring surgery for correction
-
Spondylolisthesis: A condition where vertebrae slip forward over one another, resulting in pain, nerve compression, and instability
-
Tumours: If the tumours erode the vertebrae, symptoms like pain and instability tend to occur
-
Surgical Instability Correction: Spinal Fusion Surgery may be necessary following a decompression procedure like a Laminectomy to enhance spine stability
Patients who have spondylolisthesis with discomfort in the legs and feet are often advised to have Posterolateral Lumbar Fusion. The procedure is also taken into consideration for illnesses such as disc herniation, abnormalities of the spinal curvature, such as scoliosis, and fractures or injuries to the spinal cord that significantly hamper spine stability and cause pain.
By uniting vertebrae, the process stabilises the spine to reduce pain and enhance spinal function. Before considering surgery, candidates are assessed based on the severity of their ailment, their symptoms, and how well they respond to non-surgical therapy.
A lower back incision is made before a Posterolateral Lumbar Fusion procedure to expose the vertebrae by repositioning surrounding muscles. To release pressure on the nerve roots, the lamina is removed, and any herniated discs or compressed bone fragments are removed. The sides of the spine are then stabilised with bone grafts to promote stability and fusion. Screws and rods are placed along with bone grafts in order to stabilise the spine. After that, the surgeon sutures the incision shut and covers it with a bandage to aid in healing.
Patients usually wear a plastic brace for a few weeks following Posterolateral Lumbar Fusion Surgery to provide support and limit spinal mobility. It may take several months for the fusion to heal, and symptoms may gradually get better. To rebuild mobility and strengthen muscles, physical therapy is essential.
Consult with medical professionals regularly to check on recovery and address any issues. For a good recovery and increased spinal stability, persistence and following post-operative care recommendations are crucial.
Following Posterolateral Spinal Fusion Surgery, there is an initial period of stiffness and discomfort followed by a gradual recovery. In four to six weeks, simple tasks can be resumed. A full recovery usually takes six months to a year, with physical therapy being the main focus on regaining strength and mobility.
To guarantee optimal recovery and the procedure's long-term success, patients should carefully adhere to post-operative instructions, which include adhering to mobility limitations and attending follow-up sessions.
Although Spinal Fusion Surgery is usually safe, there is a chance of blood clots, infection, and nerve injury. Additional concerns include nonunion or pseudoarthrosis, which occurs when bone fusion fails.
It is recommended that patients consult their healthcare practitioner about these risks and adhere to instructions to minimise potential adverse consequences and facilitate a successful recovery.
Physical therapy is essential for healing during the first five to nine weeks after Spinal Fusion Surgery. The goal of each session is to restore mobility and strength as the spine fuses. Progressively increasing in difficulty, activities such as walking are the first step in improving core stability and flexibility.
Patients should carefully follow their therapist's directions and refrain from physically demanding activities that might put undue strain on their developing spines. A good recovery depends on following post-operative instructions, which include limiting lifting and bending and scheduling routine follow-up visits with medical professionals.
While most patients who have Spinal Fusion Surgery experience long-term pain reduction and improved spine stability, not all patients will experience long-lasting benefits. Years after surgery, complications, including hardware problems and neighbouring segment degeneration, might cause symptoms to return. For any recurrent pain or problems to be appropriately managed and addressed, regular monitoring and follow-up with healthcare specialists are essential.
Home Dhakuria Specialities Spine-care Postero-lateral-spinal-fusion-plf

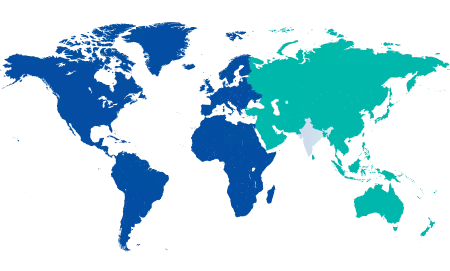
You’re on Our Indian Website
Visit the Global site for International patient services











