-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Colorectal Surgery
Colorectal Surgery Procedure in Dhakuria
The term "colorectal" combines the words colon and rectum and is often used to describe the lower digestive system, including the colon, rectum, anus, and sometimes the small intestine. Colorectal surgery refers to a wide range of procedures aimed at treating conditions affecting these areas, such as haemorrhoids, diverticulitis, and colorectal cancer. Patients with these conditions often face significant risks, including higher mortality rates, poor oncologic outcomes, and a reduced quality of life.
Many of these surgeries can be performed using minimally invasive techniques, including laparoscopic and robotic approaches, which generally offer faster recovery times and fewer complications compared to traditional open surgery. Postoperative complications, such as wound infections, haematomas, and wound dehiscence, are common after Colorectal Surgery, affecting up to 13% of patients. These complications can impact recovery and overall outcomes, making careful postoperative management essential.
FAQ's
The precise causes of colorectal cancer are unknown; however, it appears to be caused by both genetic and lifestyle factors. Cigarette smoking, a lack of physical activity, and obesity can all raise the chance of acquiring the condition. Genetic factors may predispose a person to the condition, whereas dietary and other lifestyle factors may determine which at-risk individuals get the disease. Most of the time, no clear reason is established for the development of colorectal cancer in any given individual, and it is just the result of random genetic alterations in the cells that line the colon or rectum.
Following a Proctocolectomy to remove your colon and rectum, your surgeon may join your small intestine to your anus (ileoanal anastomosis). This permits you to eliminate waste normally; however, you'll probably have numerous watery bowel movements every day.
If you are diagnosed with a big polyp or cancer, your surgeon may recommend various treatment methods, not all of which involve a major incision or cut. Our surgeons frequently perform either laparoscopic or robotic resection. This entails removing the problematic portion of the intestine and reconnecting it. For individuals with a polyp or tumour in the rectum, the surgeon may opt for Transanal Endoscopic Microsurgery, a minimally invasive approach that permits most patients to return home the same day.
When you wake up from surgery, you will be in agony and will require pain medication for a few days. You may be unable to eat for the first several days; therefore, you may be permitted to drink only small amounts of liquid since the colon requires time to heal. Most people can eat solid food in a few days.
One of the most common complications after surgery is that your intestine may not contract properly, leading to a build-up of food materials (ileus). This indicates that food and gas have difficulty travelling through your intestines. If you get an ileus, it typically lasts two to three days.
Following surgery, you should expect to spend three to five days in the hospital. Once you've passed the gas, the surgical team will usually clear you to go home. To avoid the formation of a hernia, you must avoid carrying heavy objects for six to eight weeks following surgery.
Screening tests are the most effective approach to detecting and removing polyps before they turn dangerous or to detecting cancer at an early stage when therapy is most successful. There are several screening options available. These include:
- Faecal occult blood test (FOBT)
- Flexible sigmoidoscopy
- Double-contrast barium enema
- Colonoscopy.
Patients should consult with their colorectal surgeon or other healthcare provider to determine which screening approach is best for them.
Only 5-10% of colon cancers are inherited. The most frequent hereditary form is Lynch syndrome, which is characterised by an inherited mutation in the MLH1, MSH2, MSH6, or PMS2 genes. Patients with hereditary colorectal cancer must undergo regular screening to identify the cancer early. Individuals with the following symptoms are advised to undergo regular screenings:
- Colorectal cancer appears at a young age
- Several incidences of cancer in the same person
- Multiple relatives have colorectal cancer
- Diagnosis of colorectal cancer or other associated malignancies.
The prognosis for colorectal cancer is primarily determined by the cancer's stage at the time of diagnosis. Patients with early-stage tumours are usually cured. The prognosis is worse for more advanced tumours, primarily because adjacent lymph nodes have been affected (stage III); yet, the chances of survival remain better than 50%. In contrast, the survival percentage is poorer when the cancer has already spread to distant sites (stage IV).
Early discovery and treatment can considerably improve the prognosis, with five-year survival rates ranging from approximately 90% for localised malignancies to about 15% for cancers that have spread to distant organs.
Yes. In addition to a good diet and lifestyle, colorectal cancer screening (to detect polyps or early-stage colorectal tumours before symptoms occur) is very helpful in preventing cancer from developing or raising the chances of a cure if colorectal cancer is discovered.
Home Dhakuria Specialities Surgical-gastro Colorectal-surgery

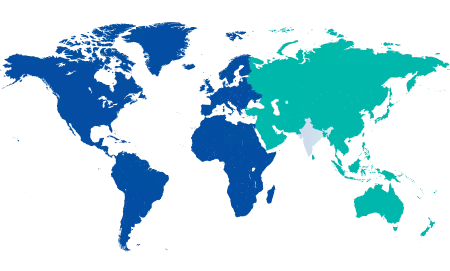
You’re on Our Indian Website
Visit the Global site for International patient services











