-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

GI Emergencies
GI Emergency Hospital in Dhakuria
Gastrointestinal illnesses and emergencies are among the most common reasons for visiting an emergency department (ED). Symptoms commonly encountered in the ED include stomach pain, nausea, vomiting, diarrhoea, and fever. GI emergencies, like other emergencies, necessitate timely measures to reduce morbidity and mortality. In contrast to other situations, it necessitates a collaborative response combining gastroenterologists, radiologists, surgeons, and critical care specialists. They also have greater hospitalisation rates than individuals who appear with non-gastrointestinal issues. Acute appendicitis (AA) is the most common cause of acute abdominal pain in children presenting to the emergency department. Emergency abdominal surgery is commonly performed when abdominal pain appears to be caused by an intestinal obstruction, a ruptured or perforated (punctured) organ, such as the stomach or appendix, a hernia with insufficient blood flow, or a blockage of blood flow.
FAQ's
Gastrointestinal (GI) bleeding occurs when there is blood in the GI system, which includes the oesophagus, stomach, small intestines, colon (large intestines), rectum, and anus. GI haemorrhage is often divided into two categories:
-
Upper GI tract: This consists of the oesophagus, stomach, and a portion of the small intestine.
-
The lower GI tract consists of the remaining small intestine, colon, rectum, and anus. Because the bleeding may be tiny, it is not usually noticeable in stool or vomit.
GI bleeding can be significant or not, depending on how much blood is lost and what is causing the bleed. Small, continual bleeding, on the other hand, might cause significant blood loss over time.
Gastrointestinal bleeding is considered life-threatening and, while usually not painful, can be fatal. To locate and treat the source of bleeding, doctors typically perform an endoscopy (an inspection of internal structures via a flexible viewing tube).
If you have severe abdominal pain, continuous vomiting, rectal bleeding, or any other troubling symptoms, seek medical assistance right away. Don't wait, especially if your symptoms are severe or worsening quickly.
Melena is a condition where patients excrete black stool with blood due to GI bleeding. Acute gastrointestinal bleeding symptoms include haematemesis, melena, and hematochezia. Bleeding that takes the patient to the doctor is a potential emergency and must be treated as such until its severity can be determined.
Patients in intensive care units (ICUs) for non-GI diseases are commonly at risk of developing gastrointestinal crises. The most prevalent causes include:
- Upper or lower gastrointestinal haemorrhage
- Acute mesenteric ischaemia
- Acute cholecystitis
- Acute pancreatitis
- Acute liver failure
Many intestinal diseases can be avoided or reduced by leading a healthy lifestyle, exercising, having excellent bowel habits, and getting examined for cancer. A colonoscopy is advised for 45-year-old patients with average risk. If you have a family history of colorectal cancer or polyps, a colonoscopy may be advised at a younger age. If you experience symptoms of colorectal cancer, contact your doctor soon. Common symptoms include:
- A change in typical bowel habits
- Blood on or in the stool might be bright or black
- Unusual abdomen or gas pain
- A very narrow stool
- A sensation that the colon has not fully emptied after passing poo.
- Unexplained weight loss
- Fatigue
- Anaemia refers to a low blood count
Treatment is determined by the specific problem and may include medication, surgery, endoscopic techniques, or a combination of these approaches. The goal is to stabilise the patient, relieve symptoms, and treat the underlying cause of the emergency.
An intestinal obstruction is considered a medical emergency, so diagnosis is usually swift. It may occur concurrently with treatment, allowing for no loss of time. The diagnosis may include:
-
Medical History: Your healthcare professional will enquire about your medical history, including any prior abdominal surgery.
-
Physical Examination: Your doctor will do a physical exam to look for enlarged abdomens or tumours.
-
They may use a stethoscope to listen for bowel noises indicating an obstruction.
-
Blood Tests: You may require a full blood count and electrolyte analysis. A blood test looks for symptoms of infection.
-
Electrolyte levels might indicate that you are very dehydrated. If so, you'll require fluids right away.
-
Imaging procedures allow your doctor to see the obstruction and check for problems. This includes:
-
Abdominal X-rays: These images can reveal the location of a blockage. These pictures may also reveal air around your intestines or diaphragm (the muscle that separates your stomach and chest). Air in these areas may suggest a dead segment of the intestine or a rupture.
-
Computed Tomography (CT) scans produce more detailed images than X-rays.
-
A barium enema X-ray is an X-ray of the colon. While you are under anaesthesia, a physician inserts a catheter (a thin tube) into your rectum. The catheter inserts a harmless liquid into your intestine, which passes through your colon while an X-ray machine collects images. The liquid makes your intestine appear more clearly on X-rays.
-
Doctors can avoid gastrointestinal bleeding by treating the underlying causes. You can avoid some of the causes of bleeding in your GI tract by treating gastro-oesophageal reflux (GER), reducing your use of nonsteroidal anti-inflammatory medicines (NSAIDs), and discussing other therapy options with your doctor.
Home Dhakuria Specialities Surgical-gastro Gi-emergencies

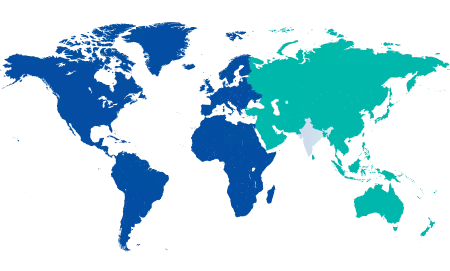
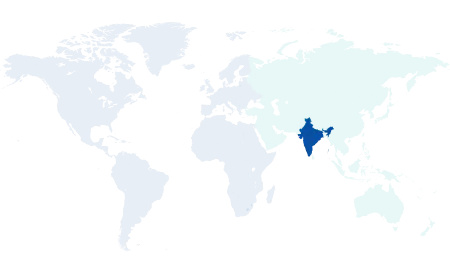
You’re on Our Indian Website
Visit the Global site for International patient services











