-
Centre of
Excellence
Centre of Excellence
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Geriatric Medicine
- GI Surgery
- Growth and Hormone
- Gynaec Oncology
- Hand Surgery
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Lifestyle Clinic
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nuclear Medicine
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Psychiatry
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Radiotherapy (Oncology Radiation)
- Renal Sciences
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
Speciality Clinics
- Doctors
- Dhakuria
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Small Bowel Resection
Small Bowel Resection Treatment in Dhakuria
The diseased or damaged portion of the small intestine is removed during a Small Intestinal Resection, and the healthy ends are rejoined (anastomosed). An Ostomy, which redirects the passage of intestinal contents to a temporary or permanent hole in the abdominal wall, may be necessary in some situations when a substantial portion of the colon is removed. This procedure helps treat intestinal blockages, tumours, diverticulitis, Crohn's disease, and ischaemic bowel disease.
Following surgery, patients usually spend time recovering in the hospital under strict observation. Long-term care may include food adjustments, prescription drugs to treat underlying illnesses, and routine check-ups with medical professionals to keep an eye on colon health and function. After Small Bowel Resection, many patients see a considerable improvement in their quality of life and symptoms with the right post-operative care and therapy.
FAQ's
Many gastrointestinal disorders, such as diverticulitis, intestinal ischaemia, bowel blockage, Crohn's disease, tumours, intestinal trauma, intestinal fistulas, and intestinal perforation, may require Small Intestine Resection. These disorders may cause severe symptoms and complications, necessitating the small intestine's afflicted section to be surgically removed. The goal of the surgery is to improve the patient's overall health and quality of life by treating the underlying disease, preventing subsequent health complications, and relieving symptoms.
Depending on the patient's health, either open or laparoscopic surgery is used to conduct Small Bowel Resection. Under general anaesthesia, the affected section is isolated and resected, and the healthy ends are connected (anastomosis) after incisions are made (big for open surgery, tiny for laparoscopic). After closing the wounds and checking for leakage, the patient is closely watched while recovering. The surgical technique is selected depending on the degree of the disease, the patient's health, and the surgeon's experience; each step is critical to the outcome.
A Small Bowel Resection can lead to several complications, including infections, anastomotic leaks, and adhesions causing obstructions. Patients might experience internal or external bleeding, nutrient malabsorption, or short bowel syndrome, resulting in diarrhoea, malnutrition, and weight loss. Incisional hernias and prolonged ileus, where the intestines temporarily stop moving, causing bloating and nausea, can also occur. Additionally, there is a risk of blood clots, such as deep vein thrombosis or pulmonary embolism. Careful monitoring and follow-up are essential to managing and mitigating these complications effectively.
Recovery time after a Small Intestinal Resection varies according to the patient's condition, surgical difficulty, and method. Typically, patients stay in the hospital for 5-7 days, with a shorter stay for laparoscopic surgeries. At-home initial recovery entails rest, a stepwise increase in exercise, and a transition from liquid to solid food intake. Appointments for follow-up are essential for tracking recuperation. Although it might take up to eight weeks, a full recovery typically takes four to six weeks.
A number of variables affect whether an Ostomy is required following a Small Bowel Resection. These include the location and size of the resection, the state of the residual colon, and the existence of infections or anastomotic leaks as a result of the surgery. The patient's general state of health and capacity for future surgeries also matter. To redirect bowel contents, an Ostomy can be necessary if reconnection of the intestine is not possible or if complications develop.
For the best possible recovery after Small Bowel Resection, post-operative care is essential. This care entails keeping wounds clean, managing pain effectively, keeping an eye out for complications, making sure the patient is eating right, escalating activity levels gradually, taking prescription drugs, scheduling follow-up appointments, and providing emotional support. Following these protocols promotes healing, lowers the chance of problems, and aids in patients' seamless recovery from Small Bowel Resection.
The long-term effects of Small Bowel Resection on intestinal function and nutritional health can be substantial. Following surgery, patients may have constipation or diarrhoea, which can alter bowel habits and interfere with the absorption of nutrients, perhaps resulting in deficiencies. Dietary changes, supplementation, or further medical care may be required, depending on the remaining bowel length and associated complications. To assess bowel function, identify weaknesses, and offer the required support for general health, healthcare practitioners must monitor patients continuously.
Dietary changes are essential to support recovery and preserve optimum health following Small Bowel Resection. Patients may benefit from eating short, frequent meals, emphasising foods high in protein, and starting with a low-fibre diet to facilitate digestion. Hydration and supplementation with vitamins and minerals may be important, along with avoiding specific foods that might increase symptoms. Dietitian advice and the gradual reintroduction of prohibited foods can help further customise meal plans for long-term health.
Following Small Bowel Resection, follow-up consultations are essential for tracking healing and taking care of any after-effects or long-term health issues. These consultations usually include evaluations of intestinal health, wound healing, nutritional condition, and drug administration. Initial sessions are more frequent and drop gradually as the patient advances in their recovery; the frequency of follow-up visits varies based on individual needs and the surgeon's recommendations.
Alternative treatment options, including Pharmacological Therapy, Endoscopic procedures, nutritional therapy, lifestyle improvements, and careful monitoring, might be considered for some illnesses instead of Small Intestinal Resections. While avoiding the dangers connected with surgery, these methods seek to control symptoms, lessen inflammation, ease strictures or blockages, maintain enough nutrition, and encourage recovery. Treatment decisions are influenced by a number of variables, including the severity of the illness, the patient's preferences, and general health. For individualised care, it is crucial to discuss choices with healthcare professionals.
Home Dhakuria Specialities Surgical-gastro Small-bowel-resection

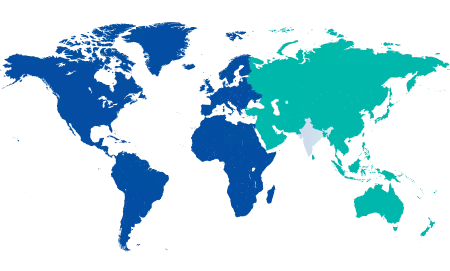
You’re on Our Indian Website
Visit the Global site for International patient services











