Heart failure occurs when the heart struggles to pump enough blood to meet the body's needs. This condition can result from weakened heart muscles, various heart conditions, or even infections. Understanding heart failure, its symptoms, causes, treatments, and preventive measures is crucial for maintaining heart health and improving quality of life.
Synopsis
What is Heart Failure?
Heart failure does not mean the heart has stopped working entirely. Instead, it signifies that the heart is not functioning efficiently, leading to the buildup of fluids in the body and potential complications in organs like the lungs, liver, and kidneys. The condition can affect either the left side, right side, or both sides of the heart.
Causes of Heart Failure
Heart failure is often a result of underlying conditions that damage or weaken the heart muscle over time. Common causes include:
-
Coronary Artery Disease (CAD): Narrowed arteries reduce blood flow to the heart, leading to damage and eventual heart failure.
-
High Blood Pressure (Hypertension): Increased blood pressure forces the heart to work harder, which can weaken it over time.
-
Cardiomyopathy: A group of diseases affecting the heart muscle, often leading to its weakening or stiffening.
-
Valvular Heart Disease: Damaged or malfunctioning valves can impair the heart's ability to pump blood effectively.
-
Myocardial Infarction (Heart Attack): A heart attack damages the heart muscle, impairing its ability to pump.
-
Congenital Heart Defects: Structural heart abnormalities present from birth may lead to heart failure later in life.
-
Diabetes: High blood sugar levels increase the risk of heart conditions that may lead to heart failure.
-
Infections: Conditions like myocarditis (inflammation of the heart muscle) can lead to heart failure if untreated.
Symptoms of Heart Failure
Heart failure symptoms can vary depending on the severity and type of the condition. Common symptoms include:
|
Symptom |
Description |
|
Worsens during physical activity or when lying down |
|
|
Fatigue and Weakness |
Reduced blood flow causes persistent fatigue |
|
Swelling (Edema) |
Fluid buildup in the legs, ankles, and feet |
|
Persistent Cough |
Chronic cough or wheezing indicating lung congestion |
|
Palpitations or irregular rhythms |
Diagnosing Heart Failure
Diagnosis typically involves a combination of the following:
-
Physical Examination: A healthcare provider may check for signs of swelling, abnormal heart sounds, or lung congestion.
-
Electrocardiogram (ECG): Measures the heart's electrical activity to detect abnormalities.
-
Echocardiogram: An ultrasound of the heart that provides detailed images of its structure and function.
-
Blood Tests: Can detect markers of heart failure, such as brain natriuretic peptide (BNP).
-
Chest X-Ray: Identifies fluid buildup in the lungs or an enlarged heart.
-
Cardiac MRI: Provides detailed images to assess the heart's structure and blood flow.
Treatment Options for Heart Failure
Treatment aims to improve symptoms, slow disease progression, and enhance quality of life. Options include:
1. Lifestyle Changes:
-
Diet: Limit salt, fat, and processed foods. Increase intake of fruits, vegetables, and lean proteins.
-
Exercise: Engage in doctor-recommended physical activities to strengthen the heart.
-
Smoking Cessation: Smoking damages blood vessels and increases heart failure risk.
-
Weight Management: Achieve and maintain a healthy weight to reduce strain on the heart.
2. Medications:
-
ACE Inhibitors and ARBs: Help relax blood vessels and reduce blood pressure.
-
Beta-Blockers: Slow the heart rate and reduce blood pressure.
-
Diuretics: Remove excess fluid to reduce swelling and lung congestion.
-
Aldosterone Antagonists: Help regulate fluid balance.
3. Medical Procedures:
-
Implantable Devices: Pacemakers and implantable cardioverter-defibrillators (ICDs) help regulate heart rhythms.
-
Angioplasty: Opens blocked arteries to improve blood flow.
-
Valve Repair or Replacement: Corrects malfunctioning valves.
-
Coronary Bypass Surgery: Improves blood flow by bypassing blocked arteries.
4. Advanced Treatments:
-
Heart Transplant: Reserved for patients with end-stage heart failure who do not respond to other treatments.
-
Left Ventricular Assist Device (LVAD): A mechanical pump that supports heart function.
Preventing Heart Failure
Prevention focuses on reducing risk factors and managing underlying conditions:
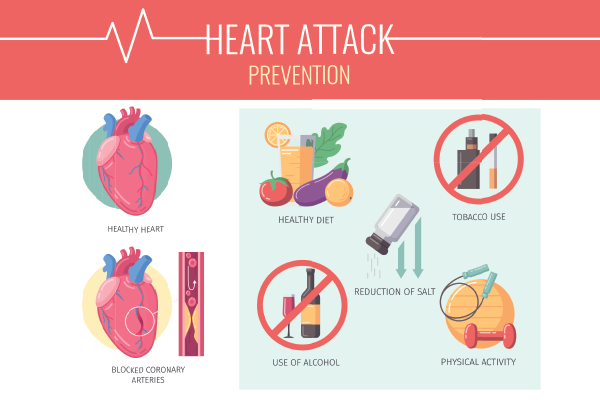
-
Control Blood Pressure: Monitor and manage hypertension with lifestyle changes or medications.
-
Manage Diabetes: Keep blood sugar levels in check with diet, exercise, and medications.
-
Healthy Diet: Follow a heart-healthy diet low in sodium, saturated fats, and added sugars.
-
Exercise Regularly: Aim for at least 30 minutes of moderate activity most days of the week.
-
Avoid Smoking: Quit smoking to improve overall cardiovascular health.
-
Limit Alcohol: Excessive alcohol intake can weaken the heart muscle.
Post-Treatment Lifestyle Changes
Patients recovering from heart failure or managing the condition long-term should adopt specific lifestyle changes:
-
Daily Monitoring: Track weight changes and report sudden increases to a healthcare provider.
-
Symptom Awareness: Be vigilant about symptoms like swelling or shortness of breath.
-
Medication Adherence: Take prescribed medications as directed without skipping doses.
-
Dietary Adjustments: Follow a low-sodium diet to prevent fluid retention.
-
Stress Management: Practice relaxation techniques like deep breathing or meditation.
Myths and Misconceptions
1. Myth: Heart failure means the heart has stopped working.
Fact: Heart failure refers to the heart's reduced efficiency, not a complete stoppage.
2. Myth: Only elderly people develop heart failure.
Fact: While more common in older adults, heart failure can affect individuals of all ages.
3. Myth: Heart failure always leads to death.
Fact: With proper management, many people with heart failure live long, active lives.
Conclusion
Heart failure is a serious condition, but early diagnosis, lifestyle changes, and appropriate treatment can improve outcomes. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to manage their heart health effectively. If you or a loved one experiences symptoms of heart failure, consult a healthcare provider for a proper diagnosis and personalized care plan.
For expert cardiac care and treatment options, visit Manipal Hospitals Ghaziabad.
FAQ's
Heart failure cannot be fully cured but can be effectively managed with lifestyle changes, medications, and medical procedures.
Diagnosis involves physical exams, ECGs, echocardiograms, blood tests, and chest X-rays.
Maintain a healthy weight, manage blood pressure, eat a balanced diet, avoid smoking, and stay physically active.
Heart failure can affect people of all ages, although it is more common in older adults.
Medications like ACE inhibitors and beta-blockers relax blood vessels, slow the heart rate, and manage symptoms effectively.





















 5 Min Read
5 Min Read