
Imagine waking up every morning, unsure if your day will be hijacked by stomach cramps, unpredictable bathroom trips, or constant bloating. For millions of people worldwide, this is the daily reality of living with Irritable Bowel Syndrome (IBS). Despite being a common digestive disorder, IBS remains misunderstood and often goes undiagnosed, leaving many struggling in silence.
The good news? IBS can be managed with the right knowledge, diet, and lifestyle adjustments. Whether you're experiencing symptoms yourself or want to help someone who is, understanding IBS symptoms and treatment is the first step toward relief. In this guide, we’ll break down the causes, triggers, and best strategies—including the IBS diet and lifestyle changes—to help you regain control of your gut health.
Synopsis
What is IBS (Irritable Bowel Syndrome)?
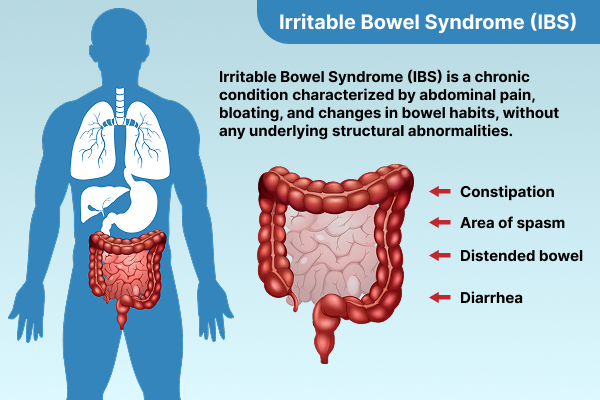
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder affecting millions worldwide. It is a chronic condition that impacts the large intestine, causing symptoms such as abdominal pain, bloating, diarrhoea, constipation, or a mix of both. While IBS does not cause permanent damage to the intestines, it can significantly impact a person's quality of life.
Symptoms of IBS
IBS symptoms and treatment vary from person to person and can range from mild to severe. The primary symptoms include:
-
Abdominal pain and cramping – Typically relieved after a bowel movement.
-
Bloating and excessive gas – A feeling of fullness or swelling in the abdomen.
-
Diarrhoea (IBS-D) – Frequent loose or watery stools.
-
Constipation (IBS-C) – Difficulty in passing stools, often hard or dry.
-
Mixed bowel habits (IBS-M) – Alternating between diarrhoea and constipation.
-
Mucus in stool – White or clear mucus present in bowel movements.
Some individuals may experience additional symptoms such as fatigue, nausea, headaches, and difficulty sleeping. Symptoms often flare up in response to specific triggers, making symptom tracking crucial for management.
Causes and Risk Factors of IBS
The exact cause of IBS remains unknown, but several factors are believed to contribute to its development:
1. Abnormal Gut Motility
Individuals with IBS may experience irregular contractions in the intestines, leading to symptoms of diarrhoea or constipation.
2. IBS Stress and Gut-Brain Connection
The gut and brain communicate through the nervous system. IBS stress and gut-brain connection play a significant role in triggering IBS symptoms, as stress, anxiety, and emotional distress can affect gut function.
3. Gut Microbiota Imbalance
An imbalance in gut bacteria can lead to digestive issues. Some studies suggest that changes in gut flora contribute to IBS symptoms.
4. Food Intolerances and Sensitivities
Certain foods, such as dairy, gluten, and high-FODMAP foods, may worsen IBS symptoms in some individuals.
5. Hormonal Fluctuations
Women are more likely to experience IBS, possibly due to hormonal influences. Symptoms often fluctuate during menstruation.
6. Infections and Post-Infectious IBS
A previous gastrointestinal infection or food poisoning can lead to the development of IBS, a condition known as post-infectious IBS.
Understanding these factors can help individuals make lifestyle changes to manage symptoms effectively.
Diagnosis of IBS
There is no specific test for diagnosing IBS, but doctors rely on clinical criteria and tests to rule out other conditions.
1. Rome IV Criteria
A diagnosis of IBS is made based on the Rome IV criteria, which include recurrent abdominal pain at least one day per week in the last three months, along with two or more of the following:
-
Pain related to defecation.
-
Changes in stool frequency.
-
Changes in stool form or appearance.
2. Tests to Rule Out Other Conditions
Doctors may conduct the following tests to ensure symptoms are not caused by other conditions:
-
Blood tests for Celiac disease and anaemia.
-
Stool tests to check for infections or inflammation.
-
Colonoscopy or endoscopy for severe symptoms.
A detailed medical history and symptom tracking are essential for an accurate diagnosis.
IBS Diet and Lifestyle Changes
1. Low FODMAP Diet
The Low FODMAP diet is one of the most effective dietary strategies for managing IBS. It involves reducing foods high in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs), which can cause bloating and discomfort. Best foods for IBS relief include:
-
Lactose-free dairy alternatives
-
Gluten-free grains
-
Lean proteins
-
Cooked vegetables like carrots and zucchini
-
Low-FODMAP fruits such as bananas and blueberries
2. Role of Fiber
Fiber intake should be tailored to IBS type:
-
For IBS-C – Increase soluble fibre (oats, bananas, carrots) to ease constipation.
-
For IBS-D – Reduce insoluble fibre (bran, raw vegetables) to prevent loose stools.
3. Hydration and Small Frequent Meals
Drinking plenty of water and eating smaller meals can help reduce bloating and discomfort.
Informational Table: IBS Triggers and Management Strategies
|
IBS Triggers |
Management Strategies |
|
Stress and Anxiety |
Meditation, deep breathing, CBT |
|
High-FODMAP Foods |
Follow a low-FODMAP diet |
|
Poor Sleep |
Maintain a consistent sleep routine |
|
Sedentary Lifestyle |
Engage in regular physical activity |
|
Food Sensitivities |
Identify and eliminate trigger foods |
|
Gut Microbiota Imbalance |
Take probiotics and maintain gut health |
Lifestyle and Behavioral Changes
1. Stress Management
Stress and anxiety can worsen IBS symptoms. Techniques such as:
-
Yoga and meditation
-
Deep breathing exercises
-
Journaling and therapy
2. Regular Exercise
Physical activity helps regulate bowel movements and reduces stress. Walking, swimming, and low-impact exercises are beneficial.
3. Adequate Sleep
Lack of sleep can exacerbate IBS symptoms. Establishing a consistent sleep routine can improve gut health.
4. Probiotics for Gut Health
Probiotics can help balance gut bacteria and reduce IBS symptoms. Foods like yoghurt, kefir, and fermented vegetables are good sources.
Medications for IBS Treatment
1. Over-the-Counter Medications
-
Antispasmodics (e.g., dicyclomine) to reduce abdominal cramping.
-
Laxatives (for IBS-C) to relieve constipation.
-
Anti-diarrheal medications (for IBS-D) to slow bowel movements.
2. Prescription Medications
-
For IBS-D: Medications like rifaximin or eluxadoline.
-
For IBS-C: Lubiprostone and linaclotide can help manage symptoms.
-
Antidepressants: Low doses of tricyclic antidepressants or SSRIs can help regulate the gut-brain axis.
3. Psychological Therapies
-
Cognitive Behavioral Therapy (CBT): Helps manage stress and gut-brain interactions.
-
Gut-Directed Hypnotherapy: Proven to alleviate IBS symptoms in some cases.
Conclusion
IBS is a complex and often misunderstood condition, but with the right knowledge and management strategies, individuals can lead a fulfilling life. Understanding IBS symptoms and treatment, identifying triggers, making dietary changes, and incorporating stress management techniques can significantly improve symptoms. Seeking medical advice and exploring medications for IBS treatment can help individuals find the best approach to managing their IBS effectively.
For expert care and treatment, visit Manipal Hospital Ghaziabad, where our specialists provide comprehensive gastrointestinal care tailored to your needs.
FAQ's
The initial symptoms of IBS often include abdominal pain, bloating, changes in bowel habits (diarrhoea, constipation, or both), and excess gas. Symptoms vary from person to person.
IBS flare-ups can be triggered by stress, certain foods (such as dairy, gluten, and high-FODMAP foods), hormonal changes, poor sleep, and infections.
There is no permanent cure for IBS, but symptoms can be effectively managed through IBS diet and lifestyle changes, stress management, and medications.
Foods that are gentle on the digestive system, such as lean proteins, lactose-free dairy, low-FODMAP vegetables, bananas, rice, and oats, can help ease IBS symptoms.
IBS stress and gut-brain connection play a significant role in symptom severity. Stress can alter gut motility and sensitivity, making symptoms worse. Stress management techniques like meditation and cognitive behavioural therapy (CBT) can help.



















 6 Min Read
6 Min Read















