
Headaches are one of the most common health complaints worldwide. They affect individuals of all ages, including children, adults, and the elderly. Headaches can significantly impact daily life, leading to missed work or school and reducing overall quality of life. While many associate severe headaches with migraines, it's essential to understand that not all headaches are migraines. Various types of headaches exist, each with distinct headache causes and treatments.
Synopsis
Understanding Migraines
Migraines are a prevalent type of primary headache disorder. Globally, about 12% of people experience migraines, with the prevalence in India around 10%. They are more common in females, especially those aged 18 to 45. Migraines are believed to result from abnormal brain responses leading to the release of pain-causing chemicals, causing swelling of brain vessels. Common triggers include stress, hormonal changes, certain foods, specific smells, or environmental factors. Genetics can also play a role, making some individuals more susceptible.
Advancements in Migraine Treatment
Recent advancements offer hope for those suffering from chronic headaches and migraines. New medications, such as triptans, gepants, ditans, and monoclonal antibodies, promise longer, pain-free periods. Procedures like greater occipital nerve blocks, Botox injections, and vagal nerve stimulation have benefited certain patients. Wearable neuromodulation devices are gaining popularity, though more research is needed to confirm their effectiveness. However, avoiding migraine triggers, maintaining a healthy lifestyle, and regular physical activity remain foundational in managing migraines.
Primary Headaches & Migraine symptoms
Not all headaches are migraines. Headaches are classified as primary and secondary headaches. Primary headaches, which are not caused by another medical condition, include tension-type headaches and cluster headaches.
Tension-Type Headaches: These are often linked to physical or mental exhaustion. They typically present as neck pain accompanied by a headache at the back of the head. Unlike migraines, they usually lack additional features like nausea or visual disturbances. Treatment may involve short courses of pain relievers and medications to relax the mind and body after proper evaluation.
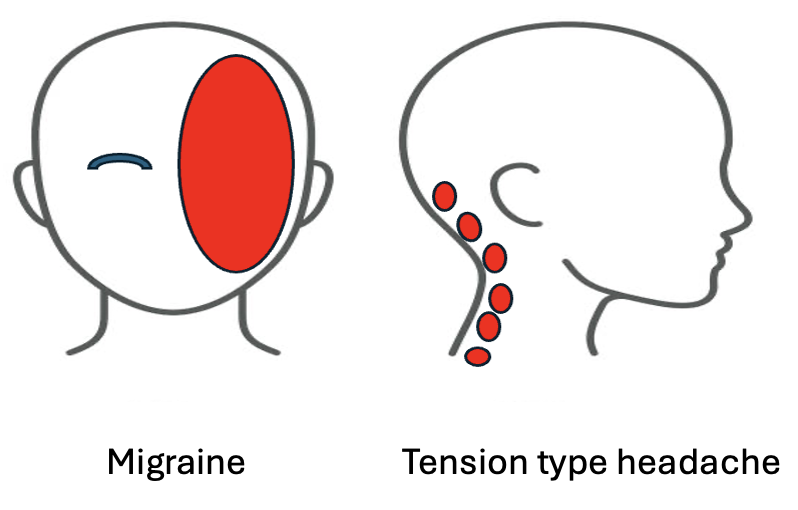
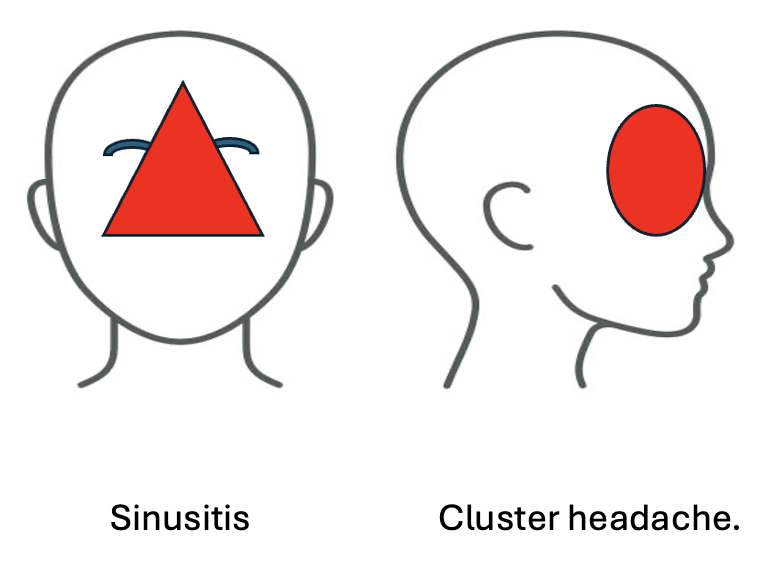
Cluster Headaches: Characterised by repeated, short-duration headaches that can occur multiple times a day. Cluster headaches are of severe intensity and often associated with redness or watering of the eyes. They are more common in younger males and may not respond to regular painkillers but often show good response to oxygen therapy. An MRI scan is typically recommended to check for issues related to the pituitary gland.
Comparison of Common Headache Types
| Headache Type | Characteristics | Triggers | Treatment Options |
| Migraine | Throbbing pain, usually on one side of the head; nausea; sensitivity to light & sound; may last hours to days | Stress, hormonal changes, certain foods, sleep disturbances | Triptans, gepants, ditans, monoclonal antibodies, Botox, nerve blocks |
| Tension-Type Headache | Dull, pressing pain, often around the forehead or back of the head; no nausea or aura | Stress, poor posture, mental exhaustion | Pain relievers, stress management, lifestyle changes |
| Cluster Headache | Severe, sharp pain around one eye; redness, watering eyes, nasal congestion; short attacks but multiple times a day | Alcohol, smoking, irregular sleep patterns | Oxygen therapy, triptans, nerve blocks, preventive medications |
| Secondary Headache | Caused by an underlying condition like high blood pressure, infections, or brain disorders; may come with red-flag symptoms | Medical conditions, medication overuse, trauma | Treating the underlying cause, urgent medical evaluation |
Recognising Secondary Headache Signs:
Secondary headaches arise due to underlying medical conditions. If not addressed promptly, they can worsen and lead to complications such as vision loss, seizures, or even require surgical intervention. Recognising the symptoms is crucial for timely evaluation, such as:
-
Systemic Symptoms: Fever, weight loss, or chills may indicate infections or systemic illnesses.
-
Neurological Symptoms: New focal neurological signs, such as weakness, numbness, or seizures, warrant immediate attention.
-
Sudden Onset: A sudden, severe headache (often described as a "thunderclap" headache) can signal a vascular issue like an aneurysm.
-
Age of Onset: New headaches in individuals over 50 are more likely to have a secondary cause.
-
Pattern Change: A significant change in headache frequency, severity, or clinical features should be evaluated.
-
Positional Headaches: Headaches that worsen with changes in posture can indicate intracranial pressure changes.
-
Precipitated by Physical Activity: Headaches triggered by activities like coughing, sneezing, or exertion may suggest an underlying structural lesion.
-
Papilledema: Swelling of the optic disc, visible during an eye examination, indicates increased intracranial pressure.
Individuals with long-term hormonal therapy, oral contraceptive use, or those with comorbidities like heart disease, obesity, diabetes, cancer, kidney, or liver disease should be vigilant, as they may have a higher risk of secondary headaches.
Tips from Neurologists
As neurologists, to manage severe headaches effectively, we recommend:
Chart Your Symptoms: Keeping a headache diary can help identify patterns and triggers, facilitating better discussions with your healthcare provider.
-
Avoid Over-the-Counter Painkillers: Frequent use can lead to medication-overuse headaches. Always consult a healthcare professional before starting any medication.
-
Watch for Red Flags: Be aware of the warning signs mentioned above and seek prompt medical attention if they occur.
-
Practice a Healthy Lifestyle: Regular exercise, a balanced diet, adequate hydration, and stress management are vital. Prevention is often the best cure.
Conclusion
Headaches are more than just migraines. They come in various forms, each with its causes and treatment approaches. Identifying your headache type, tracking symptoms, and recognising warning signs can make a significant difference in managing them effectively. Prioritising a healthy lifestyle and seeking professional medical advice when needed ensures timely intervention and better long-term outcomes. Always consult with a healthcare professional for an accurate diagnosis and tailored treatment plan if headaches persist or show unusual patterns.
FAQ's
Migraines typically involve throbbing pain on one side of the head, nausea, and sensitivity to light and sound, and they may last for hours or days.
Seek medical attention if you experience sudden, severe headaches, vision changes, persistent vomiting, unconsciousness; seizures, or headaches triggered by coughing or physical exertion.
Headaches are classified as primary (migraine, tension-type, cluster headaches) and secondary (caused by underlying conditions like infections, strokes, or high brain pressure).
Yes, stress is a major trigger for tension-type headaches and migraines. Managing stress through relaxation techniques, regular exercise, and proper sleep can help reduce headache frequency.
Yes, new medications like triptans, gepants, ditans, and monoclonal antibodies offer relief. Procedures like Botox, nerve blocks, and neuromodulation devices are also emerging options.
Yes, excessive use of painkillers can lead to medication-overuse headaches. Always consult a doctor before relying on pain medications frequently.
Migraines are often severe, pulsating, and come with nausea and light sensitivity, while tension headaches cause dull, pressure-like pain, often due to stress or fatigue.
Yes, foods like processed meats, aged cheese, caffeine, alcohol, and artificial sweeteners can trigger headaches in some people. Keeping a food diary can help identify personal triggers.
If headaches become frequent, severe, or interfere with daily life, consult a doctor. Seek urgent care if headaches come with neurological symptoms like weakness, confusion, or loss of consciousness.



















 6 Min Read
6 Min Read










