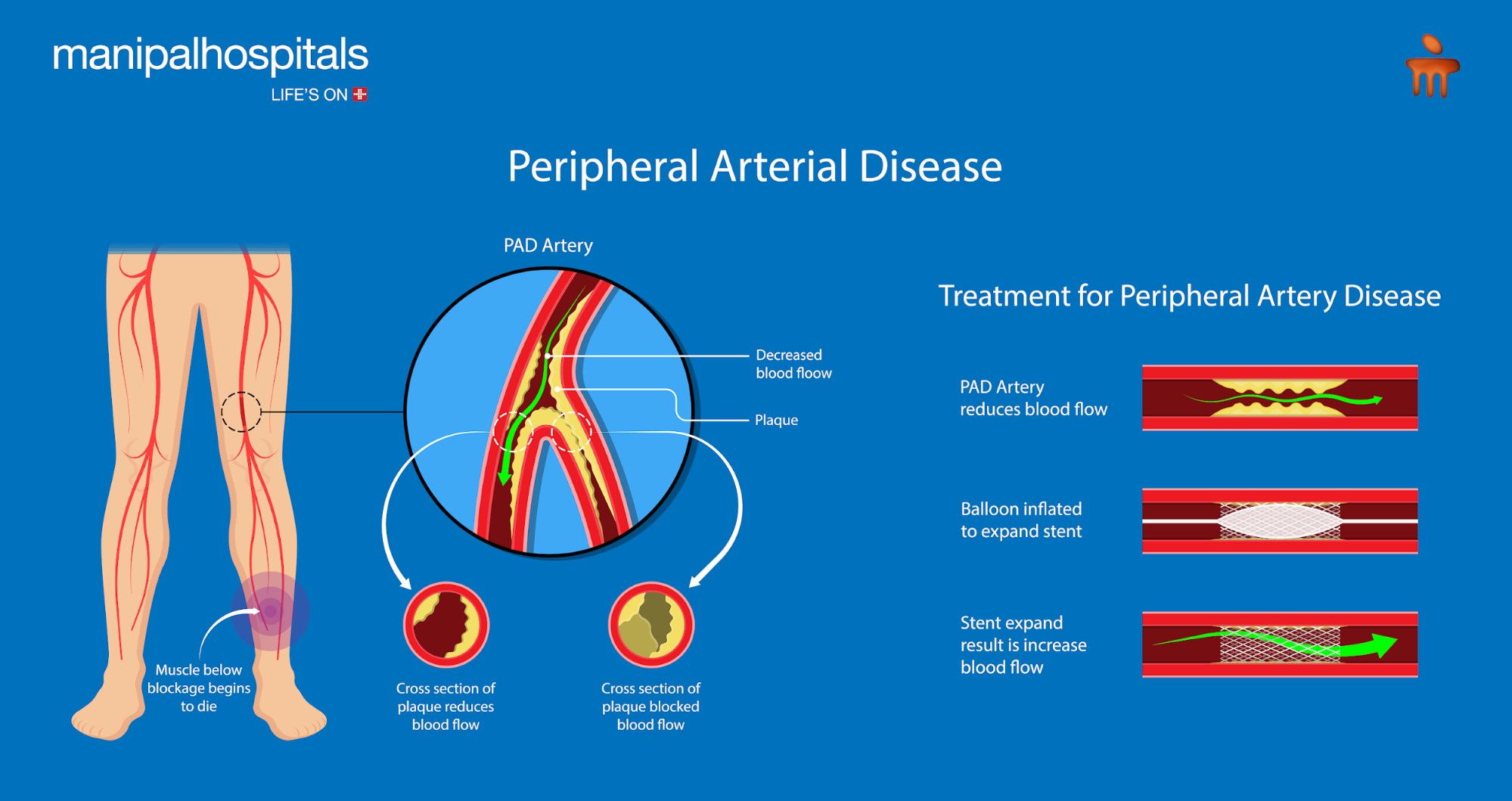
Peripheral artery disease (PAD) is associated with the disease of blood vessels (peripheral vascular system) located outside the heart and brain. These are mainly caused by the accumulation of fatty deposits within the arteries. A build-up of plaque (fats and cholesterol) in the arteries in the legs or arms is known as peripheral arterial disease, (PAD). Your blood will have a tougher time getting oxygen and nutrients to the tissues in those places as a result. Although PAD is a chronic condition, one can improve it by working out, eating less fat, and quitting smoking.
Blood flow to the arms, kidneys, stomach, and—most frequently—the legs is restricted as a result of PAD's effect on blood arteries, which causes them to constrict. African Americans are more prone than other racial groups to acquire PAD, and men are slightly more likely than women to do so. Smokers also tend to have peripheral vascular disease more frequently. Physical activity can significantly reduce symptoms, despite the condition's potentially catastrophic side effects.
What is the Cause of Peripheral Artery Disease (PAD)?
The most common cause of PAD is the accumulation of plaque within the artery wall, which reduces the flow of blood into the limbs. It also decreases the oxygen and nutrients available within the tissues. Hence, there are chances of blood clot formation within the artery wall that in turn reduces the inner size of the blood vessels while blocking the major arteries.
What are the Common Symptoms of Peripheral Artery Disease (PAD)?
Most patients do not experience any symptoms. However, due to the reduced blood flow within the arteries, any individual may experience cramps or pain in their legs. The common affected regions include the thighs, buttocks, and calves. Many people do not notice any symptoms until their arteries have narrowed by 60% or more.
Early symptoms: Intermittent claudication, which can manifest as limb discomfort, soreness, or cramping, maybe the initial sign of PAD. It mainly develops due to:
-
Regular activities
-
It vanishes with taking a rest.
-
Often returns after resuming his activities.
The discomfort could be felt in the leg as well as in the thighs or buttocks. The leg muscles may feel the following symptoms of intermittent claudication:
-
Numbness
-
Weakness
-
Heavy
-
Tiredness
Some of the advanced symptoms of Peripheral Artery Disease (PAD) include:
-
Weakness in the legs.
-
At night, a burning sensation in the feet.
-
Erectile dysfunction (mainly in diabetic men).
-
Fatigue due to some activities, such as walking.
-
Hair loss on the legs.
-
Shiny skin on the legs.
-
Delayed wound healing.
-
The slow growth of toenails.
-
Changes within the skin, such as decreased skin temperature or thin and fragile skin on the legs and feet.
Consult a top vascular surgeon if you need peripheral artery disease treatments.
How is PAD Disease Diagnosed?
A medical history and physical examination are needed for the diagnosis of PAD. Additionally, some other diagnostic tests include:
-
Angiogram.
-
Ankle-branchial index (ABI).
-
Flow studies using Doppler ultrasound.
-
Magnetic resonance angiography (MRA)
-
Exercising on a treadmill.
-
Photoplethysmography (PPG).
-
Pulse volume recording (PVR) waveform analysis.
-
Test for Reactive Hyperemia
What are the Peripheral Artery Disease Treatments?
The treatment for peripheral artery disease aims to reduce the risk of heart attack, stroke, and other problems, treat the symptoms; and stop the disease's course. The treatment includes:
-
Lifestyle modifications
To reduce risk factors, such as regular exercise, a healthy diet, and giving up smoking,
-
Aggressive management
Aggressive management of pre-existing diseases such as diabetes, hypertension, and high cholesterol that could exacerbate PAD
-
Antiplatelet drugs (blood thinners)
Antiplatelet drugs (blood thinners) which increase blood flow and medications that relax the blood vessel walls,
-
Vascular surgery
To reroute the blood flow, a bypass graft composed of a blood vessel from another region of the body or a tube made of synthetic material is inserted in the area of the blocked or constricted artery.
-
Angioplasty
To widen an artery and boost blood flow, your doctor inserts a catheter (a protruding, long hollow tube). Angioplasty procedures come in a variety of forms, including:
-
Inflatable angioplasty (a small balloon is inflated inside the blocked artery to open the blocked area).
-
Atherectomy (the blocked portion inside the artery is "shaved" away by a small instrument on the end of a catheter) (the blocked area inside the artery is "shaved" away by a tiny device on the end of a catheter).
-
A laser angioplasty (a laser is used to "vaporize" the blockage in the artery).
-
Stent (a small coil is expanded inside the blocked artery to open the blocked portion and is left in place to keep the artery open) (a tiny coil is expanded inside the blocked artery to open the blocked area and is left in place to keep the artery open).
Before undergoing angioplasty and vascular surgery, an angiography may be performed.





















 4 Min Read
4 Min Read