
Have you ever experienced ear pain, fullness, or even difficulty hearing? These symptoms could be pointing to a middle ear infection. Middle Ear Infections are common, especially in children, but they can also affect adults. In this blog, we’ll explore the signs to watch out for, the middle ear infection treatment options available, and how to prevent these infections from recurring. Keep reading to stay informed and protect your ear health!
Synopsis
- What is a Middle Ear Infection?
- Symptoms of Middle Ear Infections
- Types of Middle Ear Infections
- Causes and Risk Factors
- Diagnosis of Middle Ear Infections
- Treatment Options
- Complications if Left Untreated
- Prevention of Middle Ear Infections
- When to Seek Medical Attention
- Living with Recurring Middle Ear Infections
- Conclusion
What is a Middle Ear Infection?
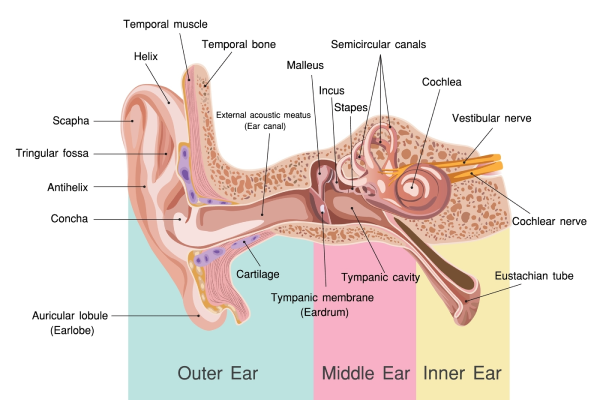
A middle ear infection, also known as otitis media, occurs when the area behind the eardrum becomes inflamed, often due to bacteria or viruses. This part of the ear plays a crucial role in transmitting sound, so any infection or fluid build-up can cause discomfort and hearing issues.
Symptoms of Middle Ear Infections
The middle ear infection symptoms can vary depending on age and the severity of the infection.
|
Symptoms in Adults |
Symptoms in Children |
|
Tugging at ears |
|
|
Hearing loss |
Fever |
|
Fluid drainage |
Crying or irritability |
|
Ear pressure/fullness |
Difficulty sleeping |
|
Dizziness or imbalance |
Young children and infants may have difficulty expressing their symptoms, so parents should watch for signs like ear tugging, irritability, or trouble feeding.
Types of Middle Ear Infections
Understanding the type of infection is essential for appropriate treatment.
-
Acute Otitis Media (AOM): A sudden and painful infection that may be accompanied by fever.
-
Otitis Media with Effusion (OME): Fluid accumulates behind the eardrum without causing infection symptoms.
-
Chronic Otitis Media: Persistent or recurring infections that can lead to complications such as hearing loss or damage to the eardrum.
Causes and Risk Factors
Middle ear infections often result from bacteria or viruses, typically following a respiratory infection. Several factors can increase the likelihood of developing an infection.
|
Causes |
Risk Factors |
|
Bacterial infections |
Cold or flu |
|
Viral infections |
Allergies |
|
Blocked Eustachian tube |
Exposure to secondhand smoke |
|
Fluid build-up |
Family history of ear issues |
The Eustachian tube, which connects the middle ear to the back of the throat, can become blocked due to inflammation or allergies. This blockage traps fluid in the ear, creating a breeding ground for bacteria and viruses.
Diagnosis of Middle Ear Infections
A healthcare provider will typically use the following methods to diagnose a middle ear infection:
-
Physical Examination: Checking for signs of redness, swelling, or fluid behind the eardrum.
-
Otoscope Use: An instrument with a light and magnifying lens is used to inspect the ear canal and eardrum.
-
Advanced Tests: Tympanometry or hearing tests may be used for more persistent or complicated cases.
Treatment Options
Middle ear infection treatment depends on the severity and type of infection.
-
Home Care: Over-the-counter pain relievers, warm compresses, and keeping the head elevated can help alleviate mild symptoms.
-
Medications:
-
Pain Relievers: Ibuprofen or acetaminophen can reduce pain and fever.
-
Antibiotics: Used if the infection is bacterial or symptoms are severe.
-
-
Surgical Procedures:
-
Tympanostomy Tubes: Small tubes inserted into the eardrum to allow fluid to drain. Recommended for chronic or recurrent infections.
-
It’s essential to follow your healthcare provider’s instructions and complete any prescribed treatments to prevent complications.
Complications if Left Untreated
If left untreated, middle ear infections can lead to:
-
Hearing Loss: Temporary or permanent hearing loss may occur, especially with chronic infections.
-
Spread of Infection: The infection may spread to nearby tissues, leading to more severe conditions such as mastoiditis.
-
Chronic Conditions: Persistent infections can cause eardrum damage or the formation of cysts.
Prevention of Middle Ear Infections
Prevention strategies can reduce the risk of developing middle ear infections:
-
Hygiene Practices: Frequent hand washing to reduce the spread of germs.
-
Vaccinations: Keeping up with flu and pneumococcal vaccines.
-
Allergy Management: Managing allergies to reduce inflammation and fluid build-up.
-
Avoiding Secondhand Smoke: Tobacco smoke irritates the Eustachian tubes and can increase infection risk.
Additionally, breastfeeding has been shown to reduce the likelihood of ear infections in infants due to the antibodies passed through breast milk.
When to Seek Medical Attention
It’s important to seek medical care if:
-
Symptoms persist for more than 48 hours.
-
There is fluid or pus drainage from the ear.
-
Significant pain or hearing loss occurs.
A healthcare provider can determine the best course of action and provide appropriate treatment.
Living with Recurring Middle Ear Infections
Chronic or recurrent ear infections can be challenging. Here are some coping strategies:
-
Follow-Up Care: Regular check-ups to monitor ear health.
-
Ear Protection: Protect ears from water exposure, especially if tympanostomy tubes are in place.
-
Support Resources: Support groups and educational resources can help families manage ongoing ear health concerns.
Conclusion
Middle ear infections can cause discomfort and even lead to complications if untreated. Early detection and proper middle ear infection treatment are key to managing these infections effectively.
If you’re experiencing ear pain or any signs of a middle ear infection, don’t wait for the symptoms to worsen. At Manipal Hospital Gurugram, our expert ENT specialists are ready to provide comprehensive care. Visit our ENT Speciality to learn more or book an appointment today to safeguard your ear health.
FAQ's
Pain, ear pressure, and mild hearing loss are common early signs.
Most infections clear up within 3-5 days, but symptoms may last longer in some cases.
No, many infections resolve on their own. Antibiotics are used if the infection is bacterial or symptoms are severe.
Yes, especially if infections are chronic or left untreated.
Doctors often use an otoscope to check for fluid behind the eardrum.
Seek medical attention if symptoms persist for more than 48 hours, if there’s fluid drainage, or if there’s significant pain or hearing loss.



















 5 Min Read
5 Min Read












