
Necrosis is a pathological process that refers to the death of cells or tissues in the body due to injury, infection, or lack of blood supply. Unlike apoptosis, which is a programmed and controlled form of cell death, necrosis typically results in inflammation and tissue damage. Understanding the types of necrosis is essential in diagnosing various medical conditions and tailoring appropriate treatment plans.
Necrosis can occur in any tissue or organ, and its impact varies depending on the underlying cause and location. Below, we will explore the different types of necrosis and how they affect various organs and tissues.
Synopsis
How Necrosis Affects Organs and Tissues
Each type of necrosis has specific implications depending on the affected tissue or organ:
-
Heart: Coagulative necrosis due to myocardial infarction leads to scar formation, reducing the heart's pumping ability.
-
Brain: Liquefactive necrosis in cerebral infarction results in permanent neurological deficits.
-
Lungs: Caseous necrosis in tuberculosis can cause respiratory failure if left untreated.
-
Pancreas: Fat necrosis can trigger acute pancreatitis, a life-threatening condition.
-
Blood Vessels: Fibrinoid necrosis increases the risk of vessel rupture and organ damage.
-
Extremities: Gangrenous necrosis may necessitate amputation if treatment is delayed.
-
Bones: Ischemic necrosis leads to joint dysfunction and chronic pain.
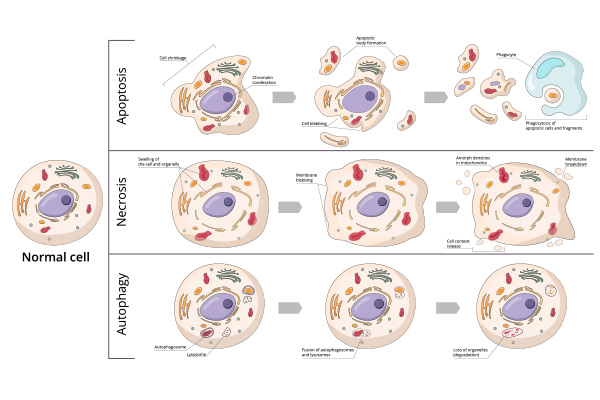
Table: Comparison of Necrosis Types
|
Type of Necrosis |
Common Sites |
Appearance |
Causes |
|
Coagulative Necrosis |
Heart, kidneys, liver |
Firm, pale |
Ischemia, infarction |
|
Liquefactive Necrosis |
Brain |
Liquid, pus-like |
Bacterial/fungal infections, stroke |
|
Caseous Necrosis |
Lungs, lymph nodes |
Cheese-like, crumbly |
Tuberculosis |
|
Fat Necrosis |
Breast, pancreas |
Chalky white deposits |
Trauma, enzymatic digestion |
|
Fibrinoid Necrosis |
Blood vessels |
Bright pink (microscopic) |
Autoimmune diseases, vasculitis |
|
Gangrenous Necrosis |
Extremities, intestines |
Black (dry), swollen (wet) |
Severe ischemia, bacterial infection |
|
Hemorrhagic Necrosis |
Intestines, lungs |
Blood-infiltrated tissue |
Venous congestion, reperfusion injury |
|
Ischemic Necrosis (AVN) |
Bones (femoral head) |
Dead bone tissue |
Loss of blood supply |
Diagnosis and Treatment of Necrosis
Diagnosing necrosis typically involves imaging studies (e.g., MRI, CT scans), blood tests, and biopsy. Treatment depends on the underlying cause and severity of tissue damage. Common treatment options include:
-
Medications: Antibiotics for infections, anticoagulants for blood clots, and anti-inflammatory drugs for autoimmune conditions.
-
Surgical Intervention: Debridement, drainage, or amputation for gangrenous necrosis.
-
Hyperbaric Oxygen Therapy: Used to promote healing in certain types of necrosis, such as gangrene.
-
Lifestyle Modifications: Controlling risk factors like diabetes and hypertension to prevent ischemic necrosis.
Preventing Necrosis
Preventing necrosis involves managing underlying conditions and maintaining good overall health:
-
Control chronic conditions like diabetes and hypertension.
-
Avoid smoking and excessive alcohol consumption.
-
Seek prompt medical attention for infections and injuries.
-
Follow a healthy diet and stay physically active to promote circulation.
Comparing Necrosis to Apoptosis: What’s the Difference?
One of the key distinctions between necrosis and apoptosis lies in the cellular processes involved. Apoptosis is a controlled process where cells die without triggering inflammation. It plays a crucial role in tissue development and immune responses.
Necrosis, on the other hand, is uncontrolled and often leads to inflammation and tissue destruction. This distinction is important because different treatments are required for conditions involving necrosis versus those involving excessive apoptosis. Understanding the underlying process helps guide therapeutic decisions.
Clinical Implications: Recognizing Necrosis Early
Early recognition of necrosis is essential for effective treatment and management. Imaging techniques such as MRI, CT scans, and ultrasound can help identify areas of necrosis. Blood tests measuring enzymes and inflammatory markers also aid in diagnosis.
Treatment strategies vary depending on the type and cause of necrosis. For ischemic necrosis, restoring blood flow through procedures like angioplasty or thrombolysis is essential. In cases of infection, antibiotics and surgical debridement may be necessary. Managing underlying conditions such as diabetes, autoimmune diseases, or hypertension is also critical to preventing further tissue damage.
Conclusion
At Manipal Hospital Gurugram, we offer comprehensive diagnostic and treatment services for conditions associated with necrosis. Our multidisciplinary team of specialists is equipped with state-of-the-art technology to provide personalized care. If you or a loved one are experiencing symptoms of necrosis or any related condition, schedule a consultation with our experts in Manipal Hospital Guruguram, today to ensure timely and effective treatment.
FAQ's
Necrosis is caused by factors such as ischemia, infections, trauma, toxins, and autoimmune reactions. Lack of oxygen and nutrient supply is a common underlying cause.
In most cases, necrosis is irreversible. However, early intervention can limit tissue damage and prevent complications.
Necrosis itself is not contagious, but the infections that cause it (e.g., tuberculosis) can be transmitted from person to person.
Diagnosis involves imaging studies, blood tests, and tissue biopsy to assess the extent and type of tissue damage.
Treatment depends on the cause and severity. Options include medications, surgical intervention, hyperbaric oxygen therapy, and lifestyle modifications.



















 5 Min Read
5 Min Read
















