
Statistics show that 3.3 million people worldwide lost their lives to intracerebral brain haemorrhage during 2021. Patients who have experienced a brain haemorrhage show a dementia risk that doubles after about 5.6 years.
In this content, a top neurosurgeon in Bengaluru discusses the causes of brain haemorrhage, its diagnostic signs, and protective measures to prevent this condition.
Synopsis
Types of Brain Haemorrhage
Brain haemorrhage represents bleeding that occurs within brain tissue and surrounding areas, which can result in brain damage. Below are the primary types:
-
Intracerebral Haemorrhage - When a brain artery ruptures, blood accumulates inside the brain tissue. High blood pressure, along with trauma, acts as the primary risk factor for brain haemorrhage. People who experience brain haemorrhage exhibit sudden weakness and speech problems and experience loss of coordination. Patients need immediate medical assistance to treat bleeding and prevent additional medical problems.
-
Subarachnoid Haemorrhage - Subarachnoid haemorrhage occurs between brain tissue and the surrounding membrane after an aneurysm ruptures. A thunderclap headache manifests after an aneurysm rupture and brings on a severe, sudden headache. Patients who experience brain aneurysm bleeding most commonly report neck stiffness alongside nausea and increased sensitivity to lights. Immediate medical assistance is warranted to stop the bleeding and lower brain pressure.
-
Subdural Haemorrhage - This bleeding occurs between brain surface tissue and the outer brain protective covering known as dura mater. The neurosurgeons most commonly diagnose this condition after patients sustain head trauma, particularly when patients are elderly. The manifestations of this condition appear gradually through symptoms like headaches, confusion, and behavioural alterations. Medical care requires continuous observation and potential brain surgery to extract accumulated blood.
-
Epidural Haemorrhage - Head injury-related bleeding most commonly forms between the skull bone and the covering dura mater after a skull fracture damages an adjacent blood vessel. The condition starts with a short blackout but immediately transitions into awareness (lucid interval) before advancing toward quick deterioration. Patients with this condition usually need urgent surgery.
Causes & Risk Factors
Understanding brain haemorrhage causes and risk factors is crucial for its prevention and timely intervention. Below are the primary causes and associated risk factors:
-
High Blood Pressure (Hypertension): Chronic hypertension weakens blood vessel walls, increasing the likelihood of rupture and bleeding within the brain.
-
Head Trauma: Injury is the most common cause of brain bleeds in people younger than age 50.
-
Blood Vessel Abnormalities: Conditions like aneurysms and arteriovenous malformations (AVMs) can lead to weakened blood vessels, increasing the risk of rupture and bleeding.
-
Blood Disorders and Anticoagulant Use: Blood disorders and the use of anticoagulant medications can increase the risk of intracerebral haemorrhage.
-
Lifestyle Factors: Excessive alcohol consumption and smoking are modifiable risk factors that can increase the likelihood of intracerebral haemorrhage.
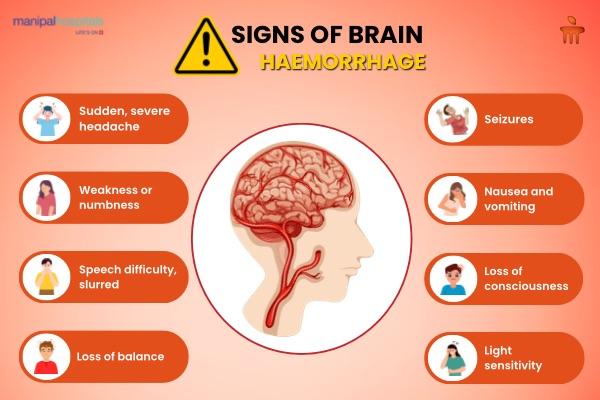
Signs & Symptoms
Recognising the signs and symptoms of a brain haemorrhage is crucial for prompt medical intervention. Symptoms can develop suddenly and may vary based on the location and severity of the bleeding. Common indicators include:
-
Sudden, Severe Headache: Often described as the worst headache ever experienced, this can signal a subarachnoid haemorrhage
-
Weakness or Numbness: A sudden tingling, weakness, numbness, or paralysis of the face, arm, or leg, especially on one side of the body
-
Vision Changes: Experiencing double vision, blurred vision, or loss of vision can occur
-
Difficulty Speaking or Understanding Speech: Sudden confusion, trouble speaking, or understanding language may be present
-
Loss of Balance or Coordination: Dizziness, difficulty walking, or loss of coordination can be symptoms
-
Nausea or Vomiting: These may accompany other neurological symptoms
-
Seizures: The onset of seizures without a prior history can indicate bleeding in the brain
-
Loss of Consciousness: Fainting or unresponsiveness may occur in severe cases
If you or someone else experiences these symptoms, especially multiple at once, seek emergency medical care immediately. Early detection and treatment are vital to improve outcomes and reduce the risk of serious complications.
Diagnosis & Medical Tests
Diagnosing brain haemorrhage is vital for effective treatment. Doctors typically perform a physical and neurological examination, followed by imaging tests. A CT scan is commonly used to detect bleeding in the brain.
An MRI can also identify brain bleeding and may be used when a CT scan doesn't provide sufficient information. Additional tests, such as a complete blood count (CBC), may be conducted to assess overall health and identify potential causes.
Treatment Options
Treating a brain haemorrhage promptly is vital to prevent further brain damage. Treatment approaches vary based on the haemorrhage's cause, location, and severity. Key treatment options include:
1. Medications
-
Blood Pressure Management: Medications are administered to control elevated blood pressure, reducing the risk of additional bleeding.
-
Reversal of Anticoagulation: For patients on blood thinners, therapies such as vitamin K or fresh frozen plasma may be used to counteract these medications and minimise further bleeding.
-
Seizure Prevention: Anti-seizure medications may be prescribed to prevent or control seizures associated with brain haemorrhages.
2. Surgical Interventions
-
Decompression Procedures: Surgeons may perform procedures like craniotomy or craniectomy to remove accumulated blood and relieve pressure on the brain.
-
Repair of Blood Vessel Abnormalities: Surgical techniques can address aneurysms or arteriovenous malformations to prevent re-bleeding.
3. Supportive Care
-
Monitoring and Stabilization: Continuous monitoring of vital signs and neurological status is essential to detect changes promptly.
-
Rehabilitation Services: Post-treatment, patients may require physical, occupational, or speech therapy to regain lost functions.
The specific treatment plan is tailored to each patient's unique condition, emphasising the importance of individualised medical care.
When to Seek Immediate Medical Help?
A brain haemorrhage is a medical emergency that requires immediate attention. Delaying treatment can lead to permanent brain damage or death. Seek emergency medical help if you or someone else experiences:
-
Sudden, Severe Headache – Especially if it feels like the worst headache ever.
-
Loss of Consciousness – Fainting, confusion, or unresponsiveness
-
Weakness or Numbness – Particularly on one side of the body
-
Difficulty Speaking or Understanding Speech – Slurred speech or trouble forming sentences
-
Seizures – A first-time seizure or an unexplained convulsion
-
Vision Problems – Blurred vision, double vision, or sudden blindness
-
Loss of Balance or Coordination – Dizziness, difficulty walking, or unexplained falls
If you notice these symptoms, call emergency services immediately. Immediate treatment improves survival and recovery chances.
Conclusion
A brain haemorrhage is a life-threatening condition that requires urgent medical attention. Understanding its causes, symptoms, and risk factors can help with early detection and prevention. Managing blood pressure, adopting a healthy lifestyle, and seeking prompt medical care can reduce risks. Spreading awareness about brain haemorrhages can save lives. Recognising symptoms early and acting fast can improve survival and recovery.
FAQ's
Chronic stress alone does not directly cause a brain haemorrhage, but it can contribute to high blood pressure, which increases the risk of brain bleeding.
Yes, a brain haemorrhage can occur anytime, including during sleep. Some people may not wake up, while others may experience symptoms like severe headaches upon waking.
Some conditions that increase the risk, like aneurysms or arteriovenous malformations (AVMs), can be hereditary. However, lifestyle factors play a major role in most cases.
Treatment can stop the bleeding and reduce complications, but recovery depends on severity. Some patients recover fully, while others may have long-term neurological effects.
Recovery varies by severity. Mild cases may improve in weeks, while severe cases may take months or years with rehabilitation for speech, movement, and cognitive skills.



















 7 Min Read
7 Min Read







.png)



