
Chronic kidney disease (CKD) affects millions of people worldwide and can progress to kidney failure if not managed effectively. When the kidneys fail to filter waste and excess fluids from the blood, dialysis becomes a lifesaving treatment. But how do you know when it's time for dialysis? In this guide, we will discuss the key signs, symptoms, and types of dialysis while emphasizing the importance of timely medical care.
Synopsis
What Are Kidneys and Why Are They Important?
Your kidneys are vital organs that perform several critical functions:
-
Filtering waste: They remove toxins and waste from the bloodstream.
-
Balancing fluids: Regulating water, salt, and electrolyte levels.
-
Hormone production: Producing hormones that control blood pressure and support red blood cell production.
When the kidneys fail to function properly, toxins and fluids build up in the body, leading to life-threatening complications. This is where dialysis steps in to perform the kidney's role.
Types of Dialysis
There are two main types of dialysis, each serving different needs:
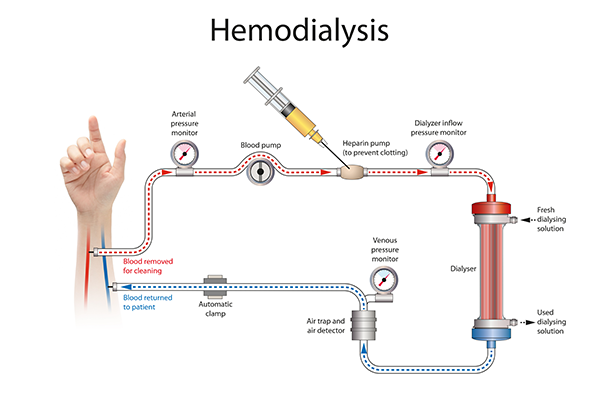
Haemodialysis (HD):
-
A machine filters waste and excess fluids from the blood.
-
Sessions typically occur three times a week at a dialysis centre or at home.
Peritoneal Dialysis (PD):
-
A cleansing fluid (dialysate) is introduced into the abdomen to absorb toxins.
-
This type is performed daily at home and can be done overnight or during the day.
Each type has its own benefits and potential drawbacks. Your healthcare provider will recommend the best option based on your condition and lifestyle.
When Do You Need Dialysis?
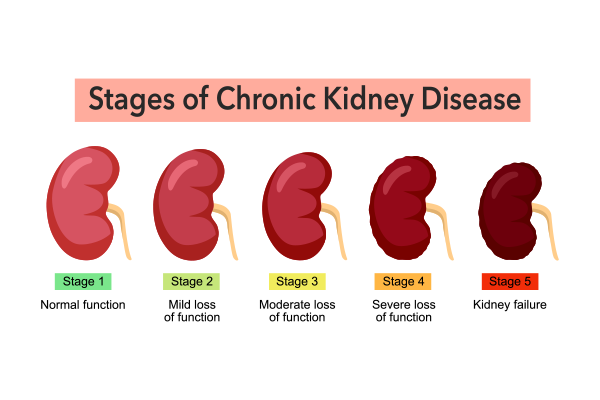
Dialysis is usually recommended when kidney function drops to 15% or less or when symptoms of kidney failure become severe. However, not everyone with reduced kidney function needs immediate dialysis. The decision depends on several factors:
-
Glomerular Filtration Rate (GFR): This test measures how well your kidneys are filtering waste. A GFR below 15 is a strong indicator for dialysis.
-
High Creatinine and BUN Levels: Elevated levels of these waste products suggest kidney dysfunction.
-
Severe Symptoms: Persistent nausea, vomiting, swelling, or fatigue may prompt early dialysis.
Importance of Dialysis: Dialysis helps remove toxins, maintain a healthy balance of electrolytes, and regulate fluid levels, preventing dangerous complications like heart failure and uremia (toxin buildup in the blood).
Signs You Might Need Dialysis
Recognising early signs of kidney failure is critical. Common symptoms that may indicate the need for dialysis include:
-
Swelling (Edema): Fluid retention in the legs, ankles, feet, or face.
-
Fatigue: Extreme tiredness due to toxin buildup and anaemia.
-
Nausea and Vomiting: Resulting from high levels of waste in the bloodstream.
-
Changes in Urine: Decreased urine output, dark or foamy urine, or frequent urination at night.
-
Shortness of Breath: Fluid buildup in the lungs can cause breathing difficulties.
-
Itching: Toxin buildup may lead to persistent, itchy skin.
-
Metallic Taste in Mouth: A common sign of uremia.
If you experience these symptoms, consult your healthcare provider immediately to evaluate kidney function.
Dialysis Side Effects
While dialysis is a lifesaving treatment, it can have side effects. These include:
-
Fatigue: Common after each session due to fluid shifts and blood pressure changes.
-
Muscle Cramps: Caused by rapid removal of fluid.
-
Infection Risk: Particularly for peritoneal dialysis patients.
-
Low Blood Pressure: A potential side effect of haemodialysis.
-
Nutritional Deficiencies: Dialysis may remove essential vitamins and minerals from the body.
Managing side effects with proper diet, medication, and regular checkups can improve the quality of life.
When to Call the Doctor
It is essential to seek a nephrologist immediately if you experience:
-
Severe or sudden swelling
-
Chest pain or shortness of breath
-
High fever or signs of infection at the dialysis site
-
Persistent nausea or vomiting
-
Severe muscle cramps or dizziness
These could be signs of complications or worsening kidney function.
How to Prevent Kidney Disease: Lifestyle Modifications
Although some causes of kidney disease (e.g., genetics) are unavoidable, lifestyle changes can help protect kidney health:
-
Manage Blood Pressure: Keep your blood pressure below 130/80 mmHg.
-
Control Blood Sugar: Diabetic patients should aim for tight blood sugar control.
-
Maintain a Healthy Weight: Obesity is a major risk factor for kidney disease.
-
Stay Hydrated: Drink plenty of water to support kidney function.
-
Avoid Excess Salt and Protein: High-sodium and high-protein diets can strain the kidneys.
-
Regular Exercise: Physical activity helps regulate blood pressure and weight.
-
Avoid Over-the-Counter Painkillers: Long-term use of NSAIDs can damage the kidneys.
Conclusion
Recognising the signs of kidney failure and seeking timely medical intervention can prevent serious complications. Dialysis plays a crucial role in managing kidney disease, and understanding the symptoms and treatment options empowers patients to take control of their health.
At Manipal Hospital Kharadi, we offer comprehensive kidney care, including advanced dialysis options and personalized treatment plans to improve your quality of life. Contact us today to learn more about our services and how we can support your kidney health.
FAQ's
There are two main types of dialysis
-
Hemodialysis: This involves passing your blood through a machine that filters it and then returns the cleaned blood to your body.
-
Peritoneal dialysis: This uses the lining of your abdomen (peritoneum) as a filter. A special solution is filled into your abdomen, where it absorbs waste products. The solution is then drained.
The frequency of dialysis depends on the type you have. Hemodialysis is typically done three times a week for several hours each session. Peritoneal dialysis can be done daily, with exchanges of the dialysis solution several times a day.
Early signs can include persistent swelling, extreme fatigue, nausea, vomiting, changes in urine output, shortness of breath, and itching. These symptoms often point to kidney dysfunction, and prompt medical evaluation is essential.
The need for dialysis is typically determined by a combination of factors such as a low glomerular filtration rate (GFR), high creatinine and BUN levels, and the presence of severe symptoms like fluid retention and uremia.
While dialysis is a life-saving treatment, it can have side effects. These can include nausea, vomiting, muscle cramps, fatigue, and changes in blood pressure. However, many of these side effects can be managed with proper care and medication after undergoing dialysis treatment.
The two main types of dialysis are haemodialysis and peritoneal dialysis. Haemodialysis uses a machine to filter the blood, usually performed at a dialysis centre or at home. Peritoneal dialysis uses the lining of the abdomen to filter waste and can be done at home either overnight or throughout the day.
Common side effects include fatigue, muscle cramps, low blood pressure, risk of infection, and nutritional deficiencies. Managing these side effects through proper diet and regular checkups can help improve overall well-being.
Yes, managing blood pressure, controlling blood sugar, maintaining a healthy weight, staying hydrated, and avoiding excessive salt or protein intake can help protect kidney health and potentially delay the need for dialysis.
Dialysis may be a long-term treatment for chronic kidney failure unless a kidney transplant is possible. For those with acute kidney failure, dialysis may be temporary until kidney function improves.



















 6 Min Read
6 Min Read




2.png)













