
Diabetes is a chronic illness that is more than just high blood sugar levels. India is considered the world’s diabetes capital, with 101 million diabetics and 136 million pre-diabetics. What is more surprising is that diabetics are twice as likely to experience strokes compared to individuals with normal blood sugar levels. Management of diabetes may reduce a huge proportion of strokes within the country. This blog explores the link between diabetes and stroke, the signs of stroke in diabetics, and the importance of effective management.
Synopsis
Types of Strokes
Strokes can be classified into two forms: ischemic and haemorrhagic. Ischemic stroke is the most common kind that occurs from blood clots in vessels that are specifically responsible for blood supply to the brain. This renders the brain clinically nonfunctional, hence producing neurological issues. In hemorrhagic strokes, a ruptured blood vessel leaks blood into the brain, damaging crucial structures.
The Deadly Duo: Diabetes and Stroke
The combination of diabetes and stroke leads to serious complications. Patients who have diabetes have 25% less favourable outcomes when it comes to regaining independent function after a stroke. Survivors experience recurrent strokes more often and may also develop vascular cognitive disabilities in the long run.
Hypertension, hyperlipidemia, and concomitant coronary or peripheral vascular disease are quite common in people with type 2 diabetes which are also independent risk factors for stroke. Impaired glucose tolerance, metabolic syndrome, and microalbuminuria are other risk factors for stroke in these populations.
What causes diabetes promotes two of the most critical complications arising from ischemic stroke: pneumonia and Deep Vein Thrombosis (DVT). The immune systems of diabetics are typically weakened, and they tend to find it hard to combat infections such as pneumonia. It also poses a higher chance of DVT due to patients' reduced mobility post-stroke.
For instance, in haemorrhagic stroke, making up 15% of the total strokes, diabetes is related to a poor outcome. Patients with diabetes in hemorrhagic strokes often have a poor outlook due to the underlying vascular condition.
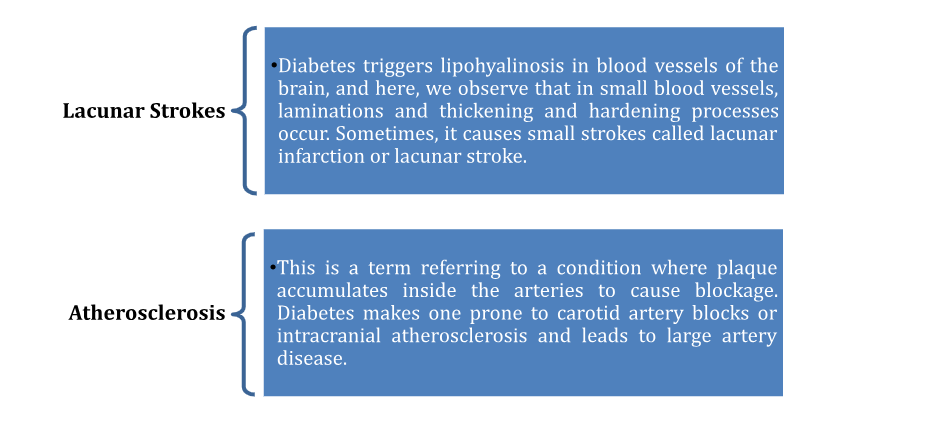
How Does Diabetes Contribute to Stroke?
Diabetes speeds up the impairment of large and small arteries and makes patients susceptible to various kinds of stroke. The two most common conditions resulting in strokes among diabetes patients are:
Symptoms of Stroke in Diabetes Patients
Common stroke symptoms include sudden facial weakness, arm or leg weakness or symptoms of low blood sugar, and slurred speech. However, in diabetic patients, these neurological signs may be masked by symptoms of low blood sugar or fatigue and high blood sugar symptoms, leading to delayed treatment and diagnosis.
Consult our neurologist in Malleshwaram if you are experiencing symptoms of diabetic stroke.
How Stroke in Diabetics Differs from Non-Diabetics?
Strokes in diabetic patients present several key differences compared to non-diabetic individuals:
-
Earlier Onset Age: Diabetic patients tend to experience strokes at a younger age.
-
Greater Severity: Strokes are often more massive in diabetic patients due to compromised blood vessel function and reduced collateral circulation in the brain.
-
Blood Sugar Fluctuations: Severe fluctuations in blood sugar levels during the acute phase of a stroke can worsen the patient's condition.
-
Complications: Diabetic patients may face additional complications, such as haemorrhaging when treated with anticoagulant drugs like tissue plasminogen activators (TPA).
-
Longer Recovery: Recovery time is often longer in diabetes patients experiencing stroke. They are known to have a 25% reduction in favourable outcomes.
Timely Intervention: Key to Managing a Stroke
For diabetic patients who are suffering from strokes, timely hospital treatment is quite essential. The less time taken after the stroke occurs, the better the chances for the patient's recovery would be.
-
Clotting Agents: Tissue plasminogen activators (TPA) are administered within a short window to dissolve blood clots in ischemic stroke patients, restoring blood flow to the brain.
-
Management of Hemorrhagic Stroke: Emergency medical services are needed to prevent further bleeding and reduce intracranial pressure, which can be fatal if not addressed swiftly.
-
Rehabilitation: Diabetic stroke patients typically require extended rehabilitation periods to recover lost physical functions.
Consult our neurology hospital in Malleshwaram if you need treatment for diabetic stroke.
Preventive Measures and Treatment
Preventing strokes in diabetic patients primarily involves achieving near-normal blood sugar levels. Other more severe measures of preventing stroke are:
-
Lifestyle Changes: A diabetic patient has to manage his lifestyle with physical activities, a proper healthy diet, and ensuring his body weight is regulated.
-
Monitoring and Treating Hypertension: High blood pressure emerges again as the key threat to the formation of both the ischemic and hemorrhagic types; you should avoid it.
-
Treating Hyperlipidemia: Hyperlipidemia should be controlled through the reduction of cholesterol in the blood through medicines, a change of diet, and exercises.
There is a well-known association between diabetes and stroke, and diabetic patients require greater vigilance than others to identify and manage stroke risks. Early intervention and lifestyle modifications are the key approaches to avoiding strokes and ensuring improved outcomes for diabetic stroke patients.
FAQ's
Diabetes results in increased risks of stroke because high blood sugar harms the blood vessels, encourages the buildup of plaques on vessel walls, and raises blood pressure. This combination can lead to inadequacy of blood supply to the brain, as found out by the studies.
Symptoms include sudden weakness in the face, arm, or leg, as well as slurred speech. Since patients with diabetes may ascribe such symptoms to low blood sugar or simply tiredness, diagnosis and treatment are sometimes delayed.
Diabetes patients may experience massive strokes which are more severe in nature. This may result in more dismal recoveries because of complications such as fluctuations in blood sugar levels, impeded healing, and higher risks of recurrence and vascular cognitive disability.



















 4 Min Read
4 Min Read














