-causes-symptoms-and-treatment.png)
Listen to article
Loading audio...
Gastrointestinal bleeding, or GI bleed, is a medical term that describes any bleeding taking place in the digestive tract, which includes the oesophagus, stomach, small intestine, large intestine, and anus. Gastrointestinal bleeding, also called intestinal bleeding or stomach bleeding, is not a disease but, instead, presents apparent symptoms of a condition that is more serious. Its high incidence rate and its potentially morbid outcome necessitate an understanding of the causes, symptoms, and diagnostic techniques, in addition to treatment for this condition.
Synopsis
- Gastrointestinal Bleeding: Types
- Causes of Gastrointestinal Bleeding
- Signs and Symptoms of GI Bleed
- When to Seek Emergency Care
- Diagnostic Methods for GI Bleed
- Treatment for GI Bleeding
- Surgical and Minimally Invasive Procedures
- Risk Factors and Prevention
- Complications of Untreated GI Bleeding
- Living with a History of GI Bleeding
- Conclusion
Gastrointestinal Bleeding: Types
The human digestive system consists of two portions: the upper GI tract (which includes the oesophagus, stomach, and duodenum) and the lower GI tract (which involves the small intestine, large intestine, rectum, and anus). Bleeding may occur in either, and its presentation usually depends upon the location and severity of the bleed.
The main types of GI bleeding include the following:
-
Overt Bleeding: Any visible bleeding, such as vomiting blood (haematemesis) or passing blood in stools (melena or hematochezia).
-
Occult Bleeding: Hidden blood loss detected through stool tests.
-
Obscure Bleeding: Difficult-to-diagnose bleeding, it is mostly found in rare conditions or lesions located in the small intestine.
Causes of Gastrointestinal Bleeding
GI bleeding can arise from several causes depending on whether the bleeding arises from the upper or lower GI tract.
Upper GI Bleed
-
Peptic Ulcers: These are sores found in the stomach or duodenum; they were probably caused by H. pylori infection or prolonged NSAID use.
-
Esophageal Varices: These dilated veins in the oesophagus (food pipe) are usually associated with liver disease, which may rupture and become a source of potentially life-threatening haemorrhage.
-
Mallory-Weiss Tears: These are tears in the esophageal lining caused by severe vomiting or retching.
-
Gastritis or Oesophagitis: An inflammation of the stomach lining or that of the oesophagus that’s usually caused by excessive alcohol use, medications, and infections.
-
Gastric Cancer: Gastric cancers can cause bleeding as they erode the stomach lining and lead to visible or hidden blood loss.
Lower GI Bleed
-
Diverticulosis: Small bulging pouches in the colon that can bleed.
-
Colitis: Inflammation of the colon caused by infections, inflammatory bowel diseases (IBD), or reduced blood flow (ischemic colitis).
-
Haemorrhoids and Anal Fissures: The common and benign causes of rectal bleeding, typically concerning straining or constipation.
-
Colorectal cancer or polyps: Malignant tumours or benign growths that bleed.
Signs and Symptoms of GI Bleed
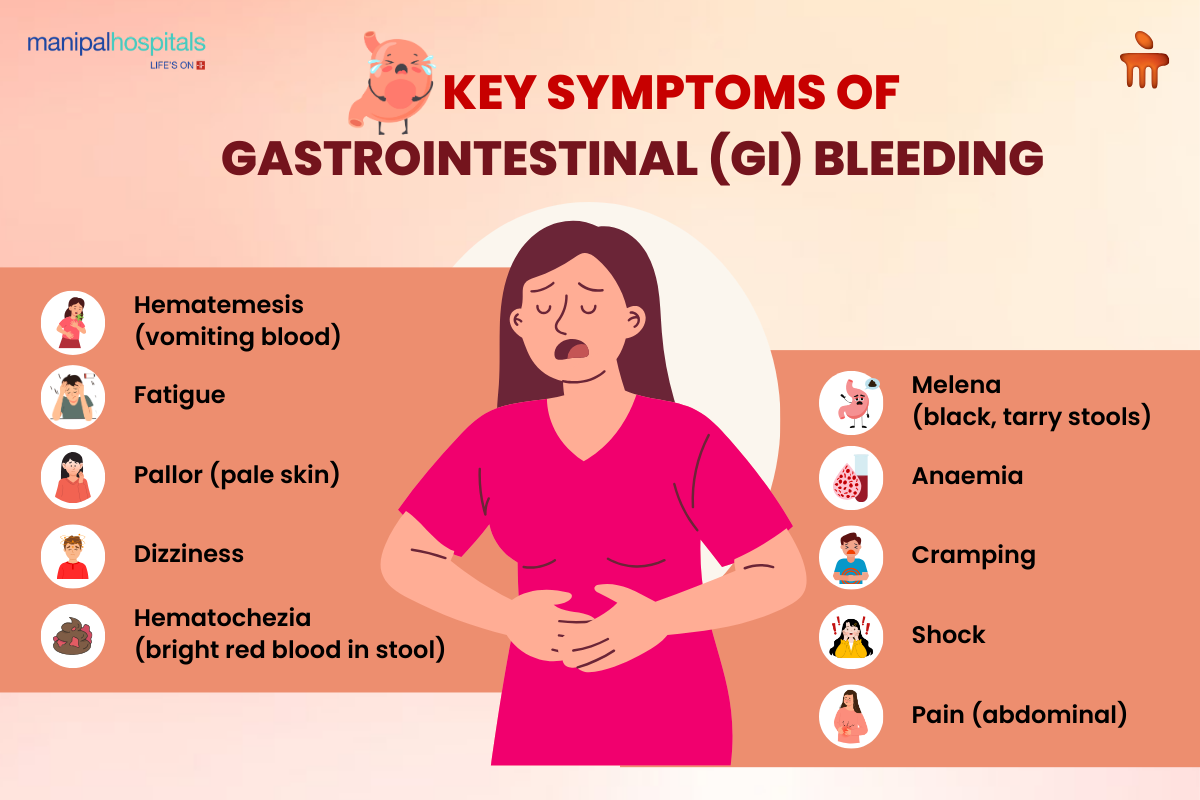
These common GI bleed symptoms may include:
-
Hematemesis (bright red blood in vomit)
-
Melena (black or tarry stools—upper GI bleeding)
-
Hematochezia (bright red blood in stool - lower GI bleeding)
-
Abdominal pain and cramping (accompanying bleeding—infectious or inflammatory conditions)
When to Seek Emergency Care
Visit an emergency room to obtain care if you experience:
-
High amounts of blood in vomiting or stool
-
Rapid heart rate or low blood pressure
-
Abdominal pain or unconsciousness
Diagnostic Methods for GI Bleed
A timely and correct diagnosis is critical for the identification of the cause of GI bleeding and the treatment approach.
Physical Examination and Medical History
Understanding what the symptoms, lifestyle factors, or past medical conditions of the patient could be to narrow down possible causes.
Endoscopy
-
Upper Endoscopy: Visualises the oesophagus, stomach, and duodenum to locate and treat bleeding sources.
-
Colonoscopy: Examines the colon and rectum for polyps, diverticula, or cancer.
Capsule Endoscopy
A swallowable camera pill is used for detecting obscure bleeding in the small intestine.
Enteroscopy
A long, flexible tube with a camera into the small intestine to visualise and treat bleeding sources that are inaccessible through upper endoscopy.
Imaging Techniques
-
CT Angiography: Helps identify active bleeding sites in complex cases
-
Radionuclide Scans: Finds bleeding by observing tagged red blood cells
Laboratory Tests
-
Complete Blood Count: Indicates anaemia and amount of blood loss.
-
Stool Tests: Detect occult blood for hidden bleeding.
Treatment for GI Bleeding
Gastrointestinal bleeding treatment is generally centred on stabilisation and the source of bleeding. Immediate interventions involve IV fluids, blood transfusions, and oxygen therapy for patients with major blood loss.
Medical Management
Medications:
-
Proton Pump Inhibitors (PPIs): Suppresses acid production in the stomach to allow healing of the ulcer.
-
Antibiotics: For infection-related diarrhoea.
-
Vasopressin: Controls bleeding in esophageal varices by constricting the blood vessel.
Surgical and Minimally Invasive Procedures
-
Endoscopic Treatments: Techniques like banding, clipping, or sclerotherapy that halt the bleeding.
-
Angiographic Embolisation: This is a minimally invasive technique of blocking the vessel responsible for haemorrhage.
-
Surgery: These are considered if life-threatening or recurrent haemorrhage recurs when other methods have failed.
Risk Factors and Prevention
Awareness of risk factors and preventive measures can greatly reduce the risk of GI bleeding.
Risk Factors
-
Chronic NSAID or aspirin use
-
Consumption of excessive alcohol
-
Smoking and poor dieting
-
Liver disease or inflammatory bowel disease
Prevention Tips
-
Regular Screening: This may be given depending on the risk of the people; for example, patients with a history of ulcers or colon polyps.
-
Trigger Avoidance: Nonsteroidal anti-inflammatory drugs (NSAIDs) and alcohol should be limited. Smoking should be stopped.
-
Underlining Conditions Must Be Treated: Effective treatment of liver disease or IBD is crucial.
Complications of Untreated GI Bleeding
Failing to treat GI bleeding symptoms early can lead to severe complications, including:
-
Anaemia: This leads to a chronic state of fatigue, weakness, and reduced quality of life.
-
Hypovolemic Shock: Excess blood supply to cause organ failure.
-
Increased Mortality Risk: Patients with relatively more complex underlying health conditions or adaptation delays will show high risks for mortality.
Living with a History of GI Bleeding
For those who have had episodes of GI bleeding, lifestyle modifications and subsequent follow-ups are important in preventing recurrences.
Dietary and Lifestyle Adjustments
-
Regular intake of a basic diet, including adequate fibre, will prevent constipation and straining.
-
Those with gastritis or ulcers should avoid foods that are spicy or acidic
-
Stay hydrated and maintain a reasonable weight
Importance of Monitoring and Support
-
Regular check-ups with a top gastroenterologist in Bangalore for monitoring against recurrence
-
Joining support groups of patients suffering from chronic GI conditions is an emotional and practical help
Conclusion
Gastrointestinal bleeding is a major life-threatening condition that should be treated urgently. Know the common GI bleed symptoms and causes and take action to seek prompt medical care. By managing the risk factors and ensuring proper preventive measures, patients can decrease their risk of having GI bleeding and other complications. Empower yourself with knowledge and prioritise your digestive health to ensure a better quality of life.
FAQ's
While stress alone doesn’t directly cause GI bleeding, it can exacerbate existing conditions like peptic ulcers or gastritis, increasing the risk of bleeding in susceptible individuals.
Bleeding in the upper GI tract often leads to vomiting blood or black, tarry stools, whereas lower GI bleeding is more likely to cause bright red blood in the stool.
Stomach Bleeding Treatment options include medication like proton pump inhibitors (PPIs), endoscopic procedures (banding or sclerotherapy), angiographic embolization, or surgery for severe or recurrent cases.



















 7 Min Read
7 Min Read











