
Meningitis is a serious and potentially life-threatening condition where the meninges, the protective membranes surrounding the brain and spinal cord, are inflamed. Spinal meningitis refers to inflammation occurring specifically in the spine. Various factors, including bacteria, viruses, fungi, parasites, and non-infectious conditions, can cause meningitis. This inflammation often manifests as symptoms like headaches, fever, and a stiff neck. Understanding the causes and associated symptoms is crucial for effective treatment and prevention.
Synopsis
What is Meningitis?
The meninges are protective brain and spinal cord coverings that provide support, structure, and cushioning against injury. They contain nerves, blood vessels, and cerebrospinal fluid. Diverse factors, including bacterial, viral, and fungal infections, can cause inflammation in the meninges, leading to meningitis. Bacterial meningitis is especially dangerous and requires immediate medical intervention.
Types of Meningitis
Based on what causes the inflammation in the meninges, there are different types of meningitis:
Viral Meningitis:
Viruses, particularly those in the enterovirus category, such as coxsackievirus A, coxsackievirus B, and echoviruses, commonly cause viral meningitis.
Bacterial Meningitis:
The most common types of bacteria that cause meningitis are:
-
Streptococcus pneumoniae, commonly found in the respiratory tract, sinuses, and nasal cavity, causes pneumococcal meningitis.
-
Neisseria meningitidis, spread through saliva and other respiratory fluids, causes meningococcal meningitis.
-
Listeria monocytogenes is a foodborne bacterium that can cause meningitis.
-
Staphylococcus aureus, typically present on the skin and in nasal passages, causes staphylococcal meningitis.
Fungal Meningitis:
Sometimes, certain fungi infect the body and spread to the brain and spinal cord, which can cause this rare type of meningitis. Individuals with weakened immune systems, such as those with cancer or HIV, are especially more susceptible.
Parasitic Meningitis:
Parasites and parasite eggs found in dirt, faeces and contaminated foods cause this non-contagious meningitis. One such parasitic meningitis is amoebic meningitis (caused by Naegleria fowleri, which enters the body through contaminated water), which is life-threatening as the causative agent may destroy brain tissue and eventually cause hallucinations and seizures.
Non-Infectious Meningitis:
This type results from underlying medical conditions like lupus, head injury, cancer, brain surgery and certain treatments and medications, not infections. It could also result from the ingestion of toxins.
Chronic Meningitis:
If the meningitis lasts longer than four weeks, it is chronic. Certain fungi, rheumatological conditions, and cancer can cause chronic meningitis.
Symptoms of Meningitis
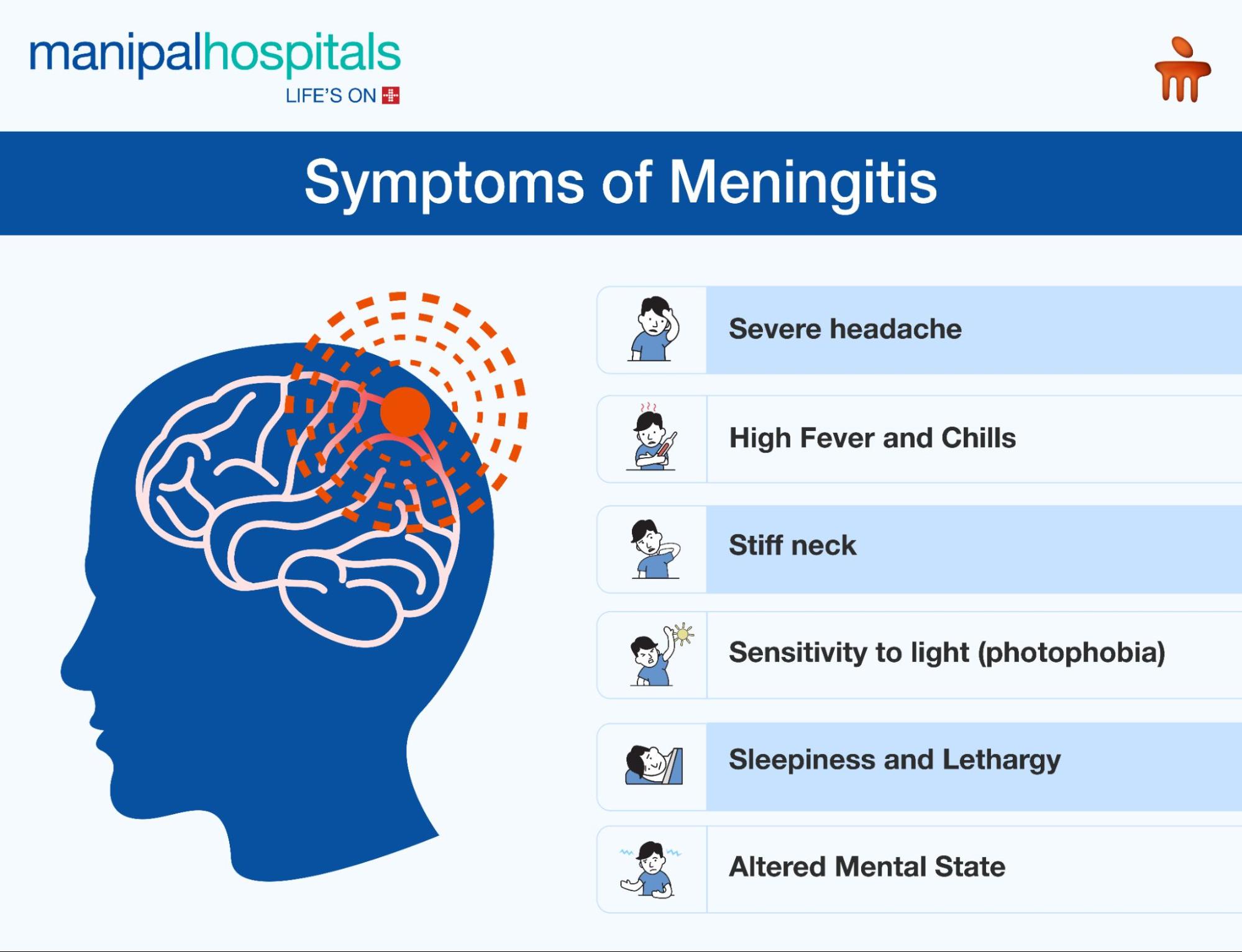
Symptoms of viral and bacterial meningitis are often similar, but bacterial meningitis is usually more severe. Some common symptoms include:
-
Severe headache
-
High fever
-
Stiff neck
-
Drowsiness, sleepiness and lethargy
-
Nausea and vomiting
-
Sensitivity to light (photophobia)
-
Confusion or altered mental state
-
Convulsions or seizures
-
Rash (especially in bacterial meningitis)
-
Decreased appetite
-
Altered Mental State
-
Chills
Symptoms can vary depending on age and cause of infection. Infants may exhibit poor feeding, respiratory symptoms, and a bulging fontanelle. If you or someone you know is showing these symptoms, seek immediate medical attention.
Risk Factors for Meningitis
Certain factors increase the risk of meningitis:
-
Age under 5 years
-
Weakened immune system (HIV, cancer, organ/bone marrow transplant, immunosuppressant medications)
-
Living in group settings
-
Cerebrospinal fluid leak
-
Absence or damage of the spleen
-
Travelling or residing in areas with a high prevalence of causative infectious diseases.
-
Chronic nose and ear infections, pneumococcal pneumonia, or widespread blood infections.
-
Head injury, traumatic brain injury (TBI), or spinal cord injury.
-
Sickle cell disease.
-
Alcohol use disorder.
Diagnosing Meningitis
The doctor may analyse the medical history and perform a physical examination to check for fever, skin issues, increased heart rate, and neck stiffness. A lumbar puncture (spinal tap) may be performed to obtain the cerebrospinal fluid. This fluid is then analysed for glucose levels, white blood cells and red blood cell count, which can help determine the type of meningitis.
Other tests may also be ordered to diagnose meningitis, such as:
-
Blood cultures identify bacteria in the blood, as some bacteria like N. meningitidis and S. pneumonia can travel from the blood to the brain.
-
A complete blood count checks the number of red and white blood cells in your blood, and elevated white blood cells indicate a meningitis infection.
-
Chest X-rays to check for tuberculosis and pneumonia, as meningitis often happens after these infections
-
A head CT scan is needed to check for brain abscess or changes in intracranial pressure.
Treating Meningitis
Treatment of meningitis usually depends on the cause:
-
Bacterial meningitis requires immediate hospitalisation to prevent brain damage and death. This type is treated with intravenous antibiotics and steroids.
-
Fungal meningitis requires antifungal agents.
-
Parasitic meningitis treatment varies, ranging from symptom management to direct infection treatment.
-
Viral meningitis may resolve by itself, but supportive care or antiviral medications may be necessary.
-
Chronic meningitis treatment addresses the underlying cause.
Prompt treatment is crucial to prevent serious complications, such as brain damage, hearing loss, or even death.
Preventing Meningitis
Preventing meningitis, particularly in high-risk individuals, relies heavily on maintaining a healthy lifestyle. Some ways include:
-
Practising good hygiene, such as frequent handwashing.
-
Avoid sharing drinks, utensils, and personal items that may carry saliva or other fluids.
-
Not smoking
-
Avoiding contact with sick people
-
Getting adequate rest
-
A healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can help strengthen your immune system.
-
Limit close contact with people who are sick, especially those with respiratory infections.
Some vaccines are available to protect against some forms of bacterial meningitis. These include:
-
Haemophilus influenzae type B (Hib) vaccine
-
Pneumococcal conjugate vaccine
-
meningococcal vaccine
Conclusion
Understanding the symptoms, causes, and prevention methods of meningitis enables the collective protection of individuals and communities. If one has concerns about oneself or a loved one, expert neurologists at the Department of Neurology at KMC Hospital, Mangalore, can provide comprehensive support for a smooth recovery.
FAQ's
aBacterial meningitis is a severe, life-threatening infection of the meninges caused by bacteria. Viral meningitis is generally less severe and often resolves on its own, caused by viruses. Bacterial meningitis requires urgent antibiotic treatment, while viral meningitis typically involves supportive care.
Meningitis can spread through close contact with an infected person, such as coughing, sneezing, kissing, or sharing utensils. Some forms of bacterial meningitis are spread through respiratory droplets.
Early symptoms can include:
-
Severe headache
-
High fever
-
Stiff neck
-
Nausea and vomiting
-
Sensitivity to light
Yes, especially bacterial meningitis. Potential complications include:
-
Hearing loss
-
Brain damage
-
Learning disabilities
-
Seizures
-
Kidney failure
-
Death
Yes, vaccines are available for some types of bacterial meningitis, including:
-
Hib (Haemophilus influenzae type b) vaccine
-
Pneumococcal vaccine
-
Meningococcal vaccine



















 7 Min Read
7 Min Read
















