
Do I have hyperthyroidism? Is it hypothyroidism? These are common questions that come into our minds when we look at our thyroid reports. This topic deals with thyroid gland dysfunction, especially hyperthyroidism.
Physiology of Hyperthyroidism
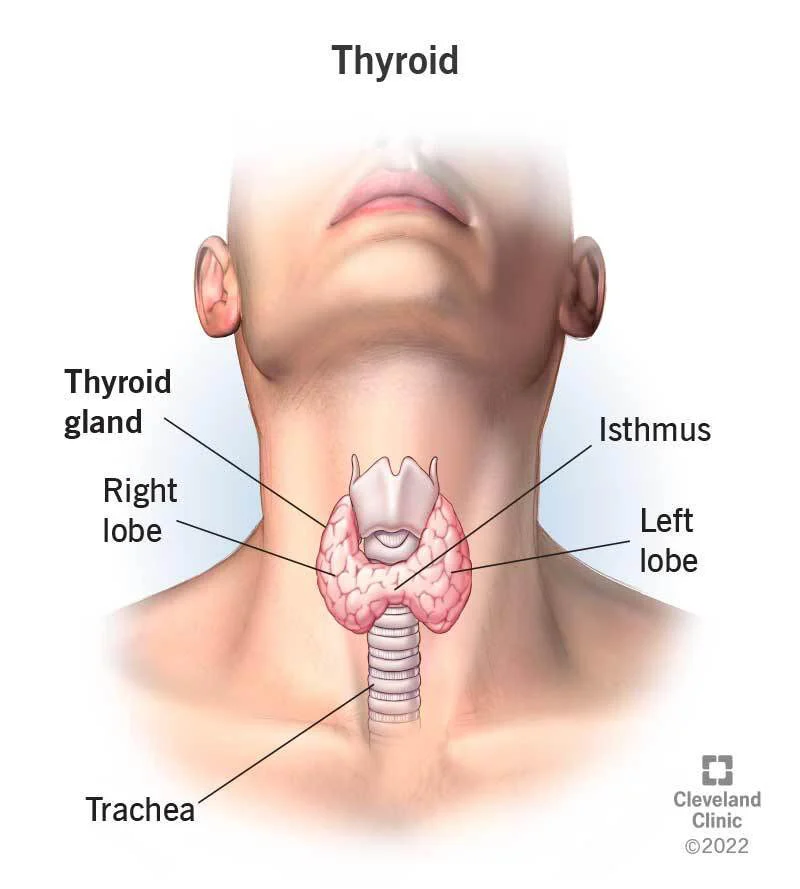
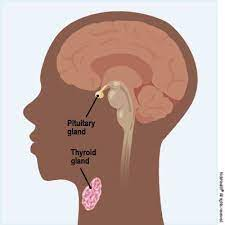
The thyroid gland is a butterfly-shaped gland which is present in the neck in front of the trachea (windpipe). The primary function of this gland is to produce thyroid hormones which are T4 and T3. The T4 hormone is produced in excess of T3, however, T4 is converted to T3 at tissue levels which is more active than T4. The thyroid hormone requires iodine, hence adequate iodine in diet is necessary to avoid diseases. The thyroid gland is in turn regulated by the pituitary-master gland (present in the brain) by producing the TSH hormone. If the T4 or T3 production is not sufficient then the TSH levels in the pituitary go up. This is seen in hypothyroidism. Similarly, if T4 / T3 levels are high, the TSH level goes down which is commonly seen in hyperthyroidism. asdocumented by the top endocrinologists in Mangalore at Manipal Hospitals.
Thyrotoxicosis / Hyperthyroidism
Even though both the terms hyperthyroidism and thyrotoxicosis are used interchangeably, both are not the same. Thyrotoxicosis is a lab finding where T4 and T3 are elevated and TSH levels are suppressed. This can be seen in hyperthyroidism, thyroiditis or overtreatment of hypothyroidism. Hyperthyroidism is a condition where the thyroid gland is over-functioning, thus producing increased levels of T4 and T3 hormones, followed by low TSH. In thyroiditis, the thyroid hormone storage of 3-6 months is released prematurely into the bloodstream in a short time leading to a similar picture (but the gland is not hyperfunctioning). Luckily hyperthyroidism is much less common than hypothyroidism. The symptoms of thyrotoxicosis are as follows:
Symptoms due to thyroid hormone excess
-
Unexplained weight loss
-
Tremors of hand
-
Palpitation- healing one’s own heartbeat
-
Increased frequency of stools
-
Generalised weakness
-
Muscle weakness
Other Symptoms
-
Goitre (thyroid swelling)
-
Eye symptoms- redness, irritation, protrusion
-
Neck pain, fever
Thyrotoxicosis can be seen due to many conditions, which are discussed below:
-
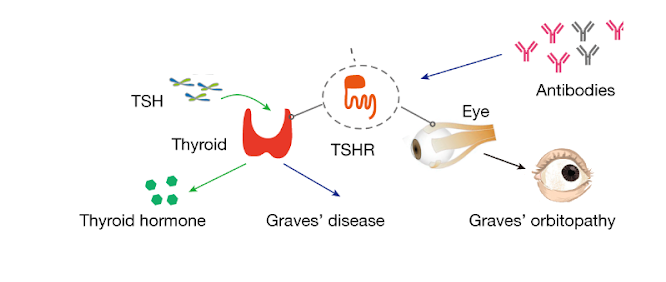
Graves’ Disease
Graves’ disease is an autoimmune disease in which auto-antibodies like TRAb (TSH receptor antibody) stimulate the thyroid to function leading to goitre, high T4 and T3; low TSH. The TRAb antibody also affects the eyes causing symptoms like redness, irritation, pain, protrusion and sometimes double vision.
-
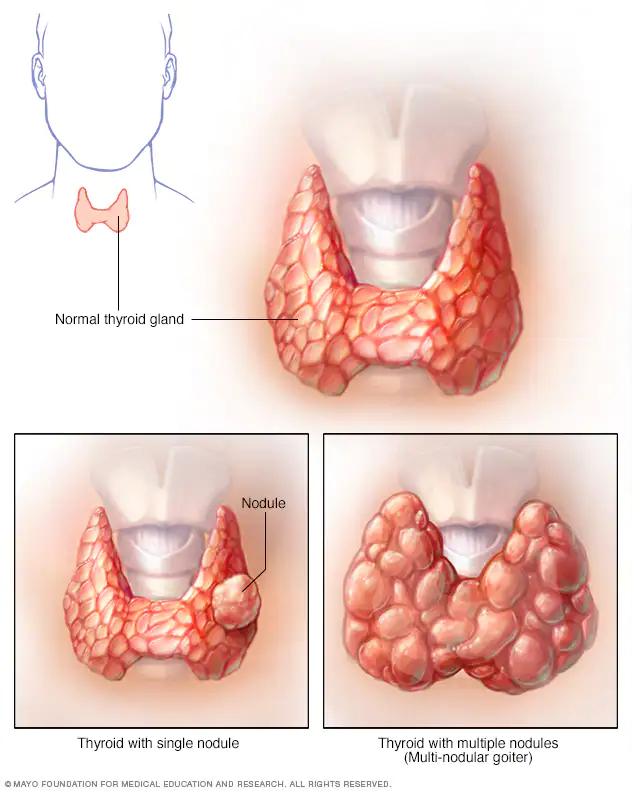
Toxic Multinodular Goitre
Subjects with long-standing goitre may sometimes develop hyperthyroidism due to autonomy (loss of regulation by the pituitary). It is usually seen in elderly patients.
-
Toxic Nodule with Hyperthyroidism
Sometimes thyroid can have a single hyperfunctioning nodule which increases thyroid hormone production. These can be diagnosed with Tc (Technetium) scan or an Iodine 123 Scan. Patients respond well to radioactive iodine ablation.
-
Thyroiditis
Patients can have a sudden release of thyroid hormone due to thyroiditis (inflammation of the thyroid gland) causing a sudden onset of symptoms like weight loss, tremors, palpitation, neck pain or fever. It is usually seen after viral infections or after delivery (postpartum thyroiditis). It is diagnosed by a combination of lab reports and clinical assessment. Patients respond well to steroids and painkillers.
-
Hyperemesis Gravidarum
Pregnant women have increased HCG hormone levels which can stimulate the thyroid leading to transient thyrotoxicosis. It is usually associated with vomiting in early pregnancy and resolves within 12 weeks.

- Other Causes
Some drugs like amiodarone, lithium, etc. can interfere with thyroid function or can interfere with lab testing giving spurious results. Other rare causes of hyperthyroidism are TSH-producing pituitary tumours and HCG-producing tumours (germ cell tumours, choriocarcinoma)
-
Investigations
-
Thyroid profile- TSH, T4 (total or free), T3 (total or free)
-
TSH receptor antibody (TRAb) - positive in Graves’ disease.
-
Tc (Technetium scan) or I123 scan- Positive in Graves, toxic multinodular goitre and toxic nodule. Negative in thyroiditis.
-
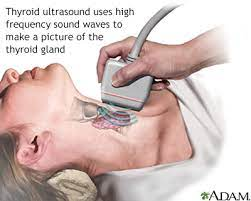
Ultrasound thyroid and FNA thyroid - in patients with nodular goitre.
-

Thyroid Management
-
Anti-thyroid drugs- Methimazole, carbimazole, Propylthiouracil
-
Medications to control symptoms and heart rate: Beta-blockers or diltiazem.
-
Radioactive iodine ablation- Patients with graves, toxic nodules, and toxic multinodular goitre can be given radioactive iodine which releases gamma radiation that kills the overactive thyroid cells making the patient hypothyroid, which can be managed more easily at an endocrinology hospital in Mangalore.
-
Surgery- in patients with large goitre, patients who are not fit for anti-thyroid drugs and radioactive iodine.
-
Steroids + anti-inflammatory drugs for patients with thyroiditis.
Follow up
Patients initially require close follow-up every 1-2 months to monitor symptoms and thyroid profiles. Once the initial control is achieved a longer interval can be prescribed. Some patients achieve long-term remission with anti-thyroid drugs. However, patients are advised against the use of anti-thyroid drugs without supervision because complications can develop in unregulated treatment.



















 7 Min Read
7 Min Read













