Every pregnant lady dreams of having a healthy baby growing in her womb following the arrival of “good news” by a positive urine pregnancy test. This expectation of the would-be mother and her family grows stronger with each day of the pregnancy and increases by leaps and bounds with every perceived movement of the fetus in the second half of the pregnancy. Unfortunately, not all pregnant mothers are lucky enough to deliver a healthy newborn. Some of the expectant mothers have a miscarriage in the early few months of pregnancy, some may be diagnosed to have subtle or lethal birth defects or anomalies in the fetus, and some end up having stillbirths due to maternal medical problems or undiagnosed structural or functional problems in the fetus.
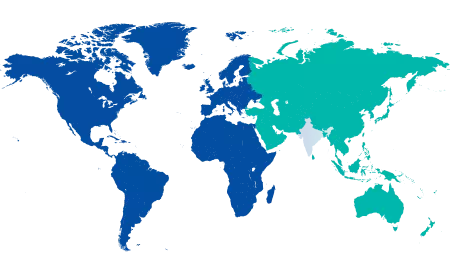
Every year, an estimated 3,03,000 newborns die due to congenital abnormalities within the first four weeks of birth around the world. Congenital anomalies can cause long-term disability, which may have a significant impact on the individual, the healthcare systems, their families, and society. The most common, severe congenital anomalies are heart defects, neural tube defects and chromosomal abnormalities like Down syndrome. As congenital anomalies may be the result of one or several genetic, nutritional, infectious, or environmental factors, it can be difficult to pinpoint the exact cause of a problem. Though not all, a few congenital anomalies can be avoided with vaccination, sufficient prenatal care, and adequate folic acid or iodine intake through fortification of staple foods or supplements.
What are Congenital Anomalies?
Congenital anomalies are also termed birth defects, congenital problems or congenital malformations. These are defined as structural or functional anomalies (metabolic disorders) that arise during intrauterine life, which are either identified prenatally, at birth or sometimes may only be detected later in infancy, such as hearing defects. In simple terms, congeniality refers to the existence/occurrence at or before birth and anomaly refers to a defect; hence, congenital anomaly means a defect present at or before birth. Although approximately 50% of all congenital anomalies cannot be linked to a specific cause, there are some known genetic, environmental and other causes or risk factors. Genes play a vital role in numerous congenital anomalies. This might be through inherited genes that code for an anomaly or resulting from rapid changes in genes called mutations. In addition, consanguinity (which simply implies that parents are related by blood) raises the chances of rare genetic congenital defects and virtually doubles the risk of neonatal and childhood death, intellectual disability, and other deformities. Low income may be an indirect determinant of congenital anomalies, due to a lack of access to sufficient, nutritional diets for pregnant women, more exposure to agents or factors such as infection and alcohol, or inferior access to health care and screening. Around 94 per cent of severe congenital abnormalities occur in low- and middle-income countries. Factors commonly linked to low income may cause or increase the incidence of abnormal prenatal development. Maternal age is also linked to poor foetal development. Advanced maternal age of more than 35 years increases the risk of chromosomal abnormalities, including Down syndrome.
Maternal exposure to certain pesticides and chemicals including certain medications, alcohol, tobacco and radiation during pregnancy may increase the risk of having a fetus or neonate affected by congenital anomalies. Working or living near waste disposal sites, smelters or mines may also be a risk factor, particularly if the mother is exposed to other environmental risk factors or nutritional deficiencies. Maternal infections like rubella and syphilis are a significant cause of congenital anomalies in low or middle-income nations. The impact of in-utero exposure to the Zika virus on the developing fetus has recently been described.
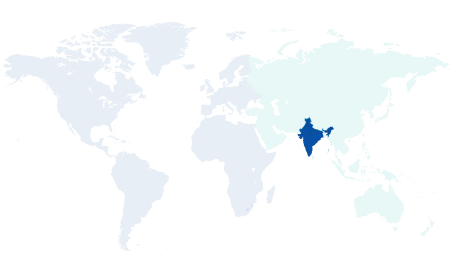
Manipal Hospitals is one of the largest and most effective prenatal care practices in the country. We have experienced and dedicated fetal medicine experts in Mangalore who take care of pregnant women through all stages of their pregnancy.
Most Important Interventions and Attempts to Reduce Congenital Defects
Preventive public health interventions aim to reduce the occurrence of certain congenital defects by removing risk factors and the reinforcement of protective factors. The most important interventions and attempts are:
-
Ensure that adolescent girls and moms have a balanced diet that includes a range of vegetables and fruit, and maintain a healthy weight.
-
Ensuring an adequate dietary intake of vitamins and minerals, particularly iron, iodine and folic acid in adolescent girls and mothers.
-
Ensuring the avoidance of harmful substances, particularly alcohol and tobacco, by expectant mothers.
-
Pregnant women (and sometimes women of childbearing age) should avoid travelling to areas where epidemics of diseases linked to congenital abnormalities are occurring.
-
During pregnancy, reduce or avoid exposure to hazardous substances in the environment (like heavy metals or pesticides).
-
Controlling diabetes before and during pregnancy through counselling, weight loss, diet, and insulin injection as needed.
-
Ensuring that any exposure of pregnant women to medications or medical radiation (such as imaging x-rays) is justified and based on a careful health risk-benefit analysis.
-
Vaccination, especially against the rubella virus, is recommended for children and women.
-
Increasing and improving the education of health care workers and others involved in congenital anomaly prevention.
-
Screening for infections, especially rubella, varicella, and syphilis, and providing appropriate treatment.
Use of the Latest Technologies to Diagnose Birth Defects
With the advent of advanced ultrasound and MRI machines and technology for diagnosing birth defects, the rates of detection of these defects have increased, which is a boon for many families and society, as it has led to an increase in discontinuation of such pregnancies. However, the sad part is that abortions are carried out even for potentially correctable defects in the fetus, like club foot or cleft lip/ palate, to name a few. Hence, there needs to be effective communication with the expectant parents to help them distinguish between potentially correctable defects and lethal defects, which shall guide them in deciding the next crucial step of continuing or discontinuing the pregnancy. Health care providers, mainly the obstetricians/sonologists, need to interact with the families and give them the needed detailed counselling regarding the scan findings and their short-term and long-term implications, quoting the current evidence.
When the clinician is unable to pinpoint the cause of the defect, it is prudent to offer the parents direct (invasive) fetal testing such as chorionic villus sampling (which is done in the first trimester) and amniocentesis/ fetal blood sampling (done in the second and third trimesters) which would help in arriving at the probable cause. These tests also have the advantage of procuring some DNA material that can be stored and used for further testing, which in turn might be of help in future pregnancies. It is also important that the parents are informed about the recurrence rate of the anomalies for future pregnancies. Even if the couple decides against invasive testing and discontinues the pregnancy, an attempt should be made to convince them to send the aborted fetus for a detailed autopsy, which will help in confirmation of the scan findings and also to diagnose other associated findings which were not picked up on ultrasound.
At Manipal Hospital, you will get help from the best team of Obstetricians and Gynaecologists in Mangalore.
Ideally, all mothers should have a minimum of 4 scans during the pregnancy, starting with an early obstetric scan between 6-10 weeks to confirm the intrauterine location of the pregnancy, to make sure the fetus is viable and to date the pregnancy. A nuchal translucency scan between 11- 14 weeks will also give an early assessment of the structural normalcy, combined with the first-trimester screening for aneuploidy, which has a sensitivity of 85-90% in detecting common chromosomal abnormalities.
Detailed Targeted imaging for Fetal anomalies (TIFFA) between 18-22 weeks, which would pick up most of the major and minor anomalies (85-90%). Fetal echocardiography can be done along with the TIFFA scan if basic cardiac screening reveals or is suspicious of a cardiac abnormality, or if there is an additional risk factor for a fetal cardiac defect, e.g., the Mother is a known diabetic, or the sibling has a cardiac defect. Lastly, an interval growth assessment between 28 - 34 completed weeks is performed to make sure the fetus is growing well for the gestational age, there is enough amniotic fluid around the fetus, and there are no evolving anomalies when compared to the TIFFA scan. An abnormal scan finding detected anytime during pregnancy, followed by detailed counselling, would help the parents by giving them the much-needed time to prepare themselves mentally, financially and socially in dealing with the problem at hand and to arrive at a conclusive decision.
The couple who had a birth defect in their previous pregnancy, the cause for which is known or unknown, should meet a Clinical geneticist with all the previous relevant records of the previous pregnancy in the pre-pregnancy period to discuss the way forward and should embark upon the next pregnancy with a positive attitude. The mother must be on Folic acid supplementation for at least 2 months before planning the next pregnancy. If the mother is not immunised for Rubella, it is advised that she get a shot of Rubella vaccine in the pre-pregnancy period and avoid pregnancy for at least one month after the vaccination, as it is a live vaccine and can have untoward effects on the fetus.
The "Global Strategy for Women's, Children's, and Adolescents' Health, 2016-2030" aspires to reach the highest attainable level of health for all women, children, and adolescents, to shape the future, and to ensure that every newborn, mother and child not only survives but also thrives well.
Manipal Hospital is one of the best gynaecology hospitals in Mangalore with highly experienced gynaecologists and obstetricians providing comprehensive gynaecology, obstetrics and congenital anomaly treatment in Mangalore.





















 3 Min Read
3 Min Read