-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Advanced Emergency Airway Management in Adults
Emergency Airway Management in Kolkata
A patient may require airway management for a range of conditions, from straightforward choking to complex airway blockages. Most frequently, foreign bodies or the tongue cause airway obstructions. It may also result from airway injuries, an increase in blood or secretions (such as mucus and saliva), or airway inflammation. Clinical symptoms such as respiratory failure, decreased awareness, sudden changes in mental state, active choking, or penetrating injuries may indicate the need for airway care. Different approaches to airway control may be used depending on the specific situation.
Airway management during emergencies involves evaluating, preparing, and sequencing medical treatments necessary to preserve or restore the breathing of a critically ill patient. Keeping the airway open ensures that air can enter the lungs from the mouth and nose.
The ability to manage airways is a crucial competency for medical professionals in life-threatening situations and is essential to emergency care practice. If emergency airway management is not performed when necessary, patients may experience low blood oxygen levels, which can be fatal.
FAQ's
When basic measures like bag-mask ventilation are insufficient, advanced emergency airway management refers to the methods and procedures utilised to establish and maintain a patient's airway. This covers procedures used to guarantee appropriate oxygenation and ventilation for severely ill or wounded individuals, such as Cricothyroidotomy, Supraglottic Airway Devices (SGAs), and Endotracheal Intubation.
As you breathe, your lungs expand and fill with air. However, when an individual develops pneumothorax, the trapped air pushes against the lungs, stopping them from expanding fully and causing them to collapse. Therefore, it causes breathing issues as the lungs cannot take in enough air.
In certain cases, advanced airway control is required for the following circumstances:
-
Despite early efforts, the patient is unable to sustain appropriate breathing or oxygenation.
-
Airway protection for coma patients or those with uncontrollable secretions (upper GI haemorrhage).
-
Airway blockage from trauma, illness, or anatomical anomalies can occur.
-
Inability to effectively oxygenate or ventilate with less invasive means.
-
In the event of an emergency surgical intervention.
-
Severe anaphylaxis or burns cause significant swelling of airway structures, leading to obstruction and necessitating airway management.
-
Emergency medical professionals expect to require airway care for an extended period, either in the emergency room or during transfer.
It is recommended to use rapid sequence intubation (RSI) to establish airway security and provide prompt access to dispense medicine or carry out diagnostic investigations.
Typical methods include:
-
Endotracheal Intubation: Creating a stable airway by inserting a tube via the mouth (or nose) into the trachea.
-
Supraglottic Airway Devices (SGAs): To keep the airway open, devices such as the King LT airway or laryngeal mask airway (LMA) are inserted above the glottis.
-
Cricothyroidotomy: When alternative approaches are ineffective or inappropriate, a Cricothyroidotomy, a surgical incision made through the skin and cricothyroid membrane to directly access the trachea, is recommended.
Usually, qualified medical professionals with backgrounds in emergency medicine, anaesthesia, or critical care administer advanced airway management. These professionals include paramedics, emergency doctors, respiratory therapists, and anaesthesiologists with specific training in airway management procedures.
Among the indications are:
-
Severe failure or discomfort in breathing.
-
Inadequate protection of the airway (e.g., trauma, altered mental condition).
-
Expected lengthy ventilation or assistance from a machine.
-
Help with medicine administration or diagnostic tests (like bronchoscopies).
Rapid and Regulated Endotracheal Intubation (RSI) is a technique used for extremely sick or wounded individuals. Usually, it includes:
-
Putting patients under sedation and neuromuscular blocking medications to make them sleep and relax their muscles.
-
Preoxygenation to provide a sufficient reserve of oxygen prior to intubation.
-
Laryngoscopy with direct visualisation of the vocal cords and endotracheal tube insertion.
-
Verification of the proper tube positioning and establishment of a secure airway with suitable ventilation.
Capnography is a useful technique for tracking the amounts of carbon dioxide (CO2) breathed during mechanical breathing and endotracheal intubation. Its responsibilities include:
-
Verification of Endotracheal Tube Insertion: The presence of CO2 in exhaled air indicates that the tube was inserted correctly, into the trachea rather than the oesophagus.
-
Monitoring the efficacy of ventilation: Continuous waveform Capnography offers feedback on ventilation in real time and aids in the detection of issues like blockage or dislodgement of tubes.
-
Evaluation of cardiac output: During resuscitation attempts, the waveform features of Capnography might help in patient evaluation by indicating changes in cardiac output and circulation condition.
Possible complications include:
-
Misplacement of the tube into the oesophagus.
-
Oral or dental injuries sustained during intubation efforts.
-
Desaturation or hypoxia occurs throughout the process.
-
Haemorrhage or damage to the airways, especially in emergency conditions or in cases where the architecture of the airways is complex.
-
Issues following intubation, such as tracheal stenosis or infections linked to the ventilator.
The effectiveness of airway management is assessed using additional tools, such as capnography and chest X-rays, alongside clinical indicators, like chest rise and listening for breath sounds on both sides, to verify correct tube placement. Once the airway is secured, the patient's breathing and oxygen levels are monitored. Care is adjusted as needed to address any issues and optimise patient outcomes.
Home Mukundapur Specialities Accident-and-emergency-care Advanced-emergency-airway-management-in-adults

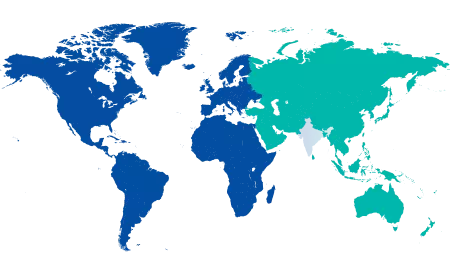
You’re on Our Indian Website
Visit the Global site for International patient services
Your Feedback is Highly Valued!











