-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Paediatric Cardiology treatments
Best Paediatric Cardiologists in Mukundapur, Kolkata
Treatments for different cardiac diseases in children include drug management, invasive procedures, and interventional approaches. Heart failure symptoms are managed by medications that control heart rhythm, and congenital problems are repaired via invasive treatments such as Cardiac Catheterisation or surgery. For certain cases, interventional cardiology treatments like Stent Insertion or Balloon Angioplasty provide non-surgical solutions.
Treatment regimens are developed by multidisciplinary teams formed with the best Paediatric Cardiologists in Mukundapur including experts such as paediatric cardiologists and cardiac surgeons. To regularly assess and manage the child's cardiac health, these plans involve follow-up care and monitoring. Lifestyle changes, such as dietary adjustments and activity guidelines, support long-term heart health. Advanced treatments like Heart Transplantation may be taken into consideration in extreme circumstances. During treatment, psychological support is crucial for the child and their family.
Home Mukundapur Specialities Cardiology Paediatric-cardiology-treatments

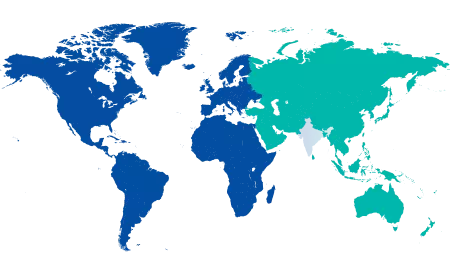
You’re on Our Indian Website
Visit the Global site for International patient services










