-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Neonatal Blood Transfusion
Neonatal Intensive Care Hospital in Mukundapur
Neonatal blood transfusion is a vital treatment for treating anaemia, blood loss, or certain disorders in infants. To verify compatibility, the process starts with blood type matching. An intravenous line is placed, and the transfusion is gradually given while the newborn's vital signs are continuously monitored to identify any unfavourable reactions. Haemolytic disorders, surgical blood loss, and anaemia associated with preterm birth are common indications. Careful management involves determining the need, getting the blood ready, and giving support for treatment. Though transfusions still entail some dangers and require careful treatment and monitoring to ensure the infant's safety and health, advances in newborn care have improved outcomes. If you are looking for Neonatal blood transfusion in Mukundapur, Manipal Hospitals is the place to go.
FAQ's
When a newborn receives a blood transfusion, an intravenous line is inserted, the baby's blood type is carefully matched to the donor blood, and the blood is slowly given while the baby's vital signs are monitored. Usually, anaemia, blood loss, or certain medical disorders are treated with it, and any adverse reactions are closely monitored.
All of the body's tissues receive oxygen from red blood cells. An infant is diagnosed with anaemia if their red blood cell count (haematocrit) is abnormally low. Neonates who suffer from anaemia either have blood loss or are unable to generate the necessary amount of blood. Over time, red blood cells gradually deteriorate and must be replenished. It may be challenging for premature babies to produce enough red blood cells to meet their requirements. Small amounts of blood may also be lost over time when blood is taken for essential laboratory testing. All of these causes of anaemia are more common in infants born before 28 weeks of pregnancy. Therefore, blood transfusion in neonates helps restore adequate red blood cells.
Since oxygen is necessary for all body organs to operate, red blood cells play a vital role in the transportation of oxygen throughout the body. Anaemic babies appear paler and sleepier than usual. Babies with anaemia may find it difficult to eat, and some may experience severe breathing problems.
Iron supplements can be given to babies orally or through their feeding tube as early as two weeks of age. A red blood cell transfusion is necessary if an infant is exhibiting symptoms, has a low haemoglobin level, or needs surgery.
Other than red blood cells, certain neonates require transfusions of blood components that are administered under highly precise circumstances. Other blood components that may require transfusions rarely include
-
Platelets: Platelets are blood cells that aid in stopping and preventing bleeding. Your infant will receive a platelet transfusion if they are bleeding severely or have a low platelet count and are in urgent danger of bleeding further.
-
Plasma: The yellow liquid enveloping platelets and red blood cells is called plasma. It includes components that promote blood clotting.
Transfusions can undoubtedly save lives when used to treat patients with extreme blood loss or shock. Other advantages that might not be as evident are as follows:
-
Early discharge from the NICU
-
Better feeding
-
Reduced apnoea, or the disruption of breathing
-
Reduced respiratory distress
-
Reduced brain injury (caused by insufficient oxygen)
Blood transfusions carry minimal risk because of thorough screening protocols. The risks include blood-related issues, allergic reactions, infections, and issues related to blood volume.
-
Possibility of infection: Blood can spread viruses, including HIV, hepatitis C, and hepatitis B. Blood donors are only permitted to donate if they do not have any risk factors for any of these infections. Donated blood is also thoroughly examined for these infections. If donated blood tests positive for the hepatitis or HIV viruses, it is not accepted. There is very little chance that the blood used for a transfusion would harbour one of these viruses.
-
The possibility of an allergic response: In infants, the chance of an allergic reaction to blood is minimal. However, a baby receiving red blood cells could have their body reject them due to an allergic reaction. Haemolysis is the term for this. A rash or fever is the result of a transfusion. Blood recipients' babies are routinely observed for any indications of allergies.
-
Issues related to blood volume: Introducing red blood cells causes the baby's body's fluid content to rise. Some infants may find it difficult to manage the additional fluid. A medicine can be administered to these babies to aid in the removal of excess fluids from their urine.
Managing the associated risks when dealing with neonates is crucial, and the below guidelines can help in managing them:
-
Careful selection of donors is necessary to minimise the possibility of unfavourable reactions.
-
Before transfusion, compatibility tests and blood type matching should be done.
-
Administering blood gradually and monitoring for any adverse reactions.
-
Strictly adhering to aseptic procedures during transfusion to avoid infections.
-
Monitoring vitals during transfusion.
-
Being ready to handle any complications such as haemolysis, fluid overload, or respiratory distress as soon as they arise.
Home Mukundapur Specialities Neonatology-nicu Neonatal-blood-transfusion-2

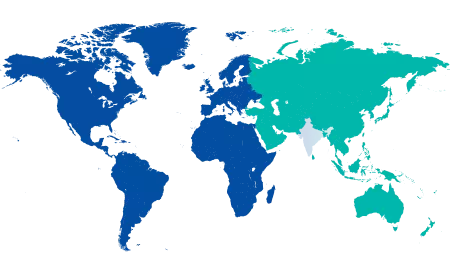
You’re on Our Indian Website
Visit the Global site for International patient services










