-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Transplant Medicine
Organ Transplant Hospital in Mukundapur
Transplant medicine is dedicated to organ and tissue transplantation. In addition to ensuring compatibility, avoiding rejection, and handling complications, it also involves managing patients before, during, and following transplantation. Kidney, liver, heart, lung, and bone marrow transplants are important aspects of care in Transplant Medicine. Transplant medicine in Mukundapur integrates immunology, pharmacology, and surgery. To support the immune system in battling infection and avoiding rejection of the transplanted organ, it will be necessary to take medication. This delicate equilibrium must be managed with great care, as rejection occurs when the immune system sees the new organ as an invader and attacks it.
Immunosuppressive drugs are those that work by preventing the immune system from harming the newly implanted organ. But they also make it more difficult for the immune system to combat actual threats like bacteria, fungus, and viruses, which increases your chance of infection. Anti-rejection drugs minimise side effects and effectively inhibit the immune system by acting on distinct stages of the immunological response. Three stages are often characterised as clinical immunosuppression: induction, maintenance, and anti-rejection.
FAQ's
Receiving an organ transplant improves your quality of life. To extend the life of the newly acquired organ as much as possible, one should look after oneself. One of the most crucial aspects of caring for yourself and the newly acquired organ is taking your transplant medications on schedule every day. You should experience fewer side effects and other issues if you take your transplant medications as prescribed. All of the medications that your physician recommends are critical to both your overall health and the health of your growing organs. Without your doctor's advice, stopping any of the medications or even missing a single dosage could be harmful.
Using drugs to suppress the recipient's immune system after organ transplantation is known as post-transplant immunosuppression. Lowering the immunological reaction prevents the transplanted organ from being rejected. Immunosuppressive medications, including antimetabolites, calcineurin inhibitors, and corticosteroids, are frequently prescribed based on the patient's risk of rejection and specific requirements.
There are three approaches to suppressing the immune system after a transplant.
-
Induction immunosuppression: The goal of this approach is to prevent acute rejection by administering all drugs at increased doses quickly after transplantation. These drugs are continued for 30 days after discharge; they cannot be used on a long-term basis for immunosuppressive maintenance.
-
Maintenance immunosuppression: All immunosuppressive drugs used before, during, or following a transplant with the goal of long-term maintenance are referred to as maintenance immunosuppression.
-
Anti-rejection immunosuppression: All immunosuppressive drugs administered to treat an acute rejection event during the initial post-transplant period or a designated follow-up period, which typically lasts up to 30 days following the diagnosis of acute rejection, are included in this method.
The amount of transplant medication in a patient's body varies and can be influenced by factors such as the type of organ transplant and how the medicine is taken, whether with or without food. Blood tests can determine the level of medication in the body and help the transplant team determine if the patient is receiving the correct dosage.
The most often given immunosuppressants are prednisolone, mycophenolate, and tacrolimus.
-
Tacrolimus: It must be taken once or twice daily. Tremor, hair loss, headaches, sleep disturbances, diabetes, and poor kidney function are some of the side effects. Tacrolimus blood levels will be closely monitored to minimise adverse consequences.
-
Mycophenolate: It is prescribed to some patients. The doctors will explain why mycophenolate is necessary if you need to take it. You must take it twice a day. Nausea and diarrhoea are side effects. Additionally, it may have an impact on blood counts, particularly white cell counts.
-
Prednisolone: After the transplant, the majority of patients take prednisolone for a short time. The doctor will take a call if you need to take it for longer than a week. Indigestion, increased hunger, weight gain, elevated blood pressure, elevated blood sugar, and mood swings are some of the side effects.
After undergoing a transplant, as the patient is more susceptible to infections, your healthcare provider may recommend taking some vaccinations to protect your overall health and the transplanted organ. Some of the vaccinations include:
-
Annual seasonal influenza vaccination
-
Pneumococcal immunisation every 5 years
-
COVID-19 vaccination per federal regulations
-
Shingles vaccination (non-live) if you are older than 70
Immunosuppressants decrease the possibility that your body will reject donated organs. However, there can be dangers or difficulties, like:
Dosages missing
You must take immunosuppressants according to your doctor's instructions. Missing doses raise the chances that your body will reject donor organs.
Increased risk of infection
Medicines suppress the immune system and make the body more susceptible to infections. This raises your chance of contracting potentially fatal diseases like:
-
Blood infections such as sepsis
-
Fungal diseases, such as skin infections and thrush, have a widespread impact on numerous individuals
-
Skin infections such as cellulitis
You will need to take immunosuppressive (anti-rejection) medications following an organ transplant. By preventing your immune system from fighting (or "rejecting") the donor organ, these medications assist you. They usually have to be taken for the duration of the time that your transplanted organ is functioning.
Home Mukundapur Specialities Nephrology Transplant-medicine-2

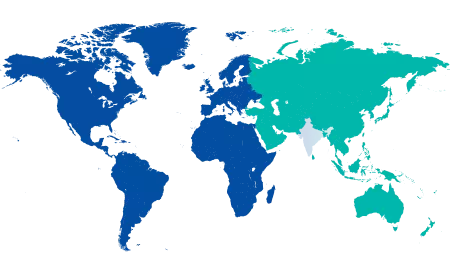
You’re on Our Indian Website
Visit the Global site for International patient services










