-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Fibroid Clinic
Fibroid Treatment in Mukundapur
Non-cancerous growths found in or on the surface of the uterus are called uterine fibroids. These frequent cysts can cause excessive menstrual bleeding, pelvic pain, frequent urination, and problems during pregnancy. Although not all fibroids need treatment, doctors can adequately address the cause of the problem or health issues with appropriate care and treatment.
At Manipal Hospitals, Mukundapur, Kolkata, our Obstetrics and Gynaecology Department provides care and treatment for fibroids exclusively in our dedicated fibroid clinic. We use advanced imaging techniques for accurate diagnosis and personalised treatment plans. These include minimally invasive procedures such as Laparoscopic and Hysteroscopic Myomectomy, as well as Uterine Artery Embolisation. Our modern facilities and experienced surgeons ensure you receive the best possible care. We focus on your comfort and well-being, providing support throughout your healing journey. At Manipal Hospitals, Mukundapur, we are committed to helping you manage your symptoms and improve your overall well-being with compassionate and expert care.
FAQ's
Fibroids are benign (non-cancerous) tumours that grow inside the uterine muscle wall. They are also referred to as uterine leiomyomas or myomas. They are made up of fibrous connective tissue and smooth muscle cells. Fibroids can range in size, shape, and number, from small growths resembling seeds to massive masses that can change the uterine shape. They can develop anywhere within the uterine wall: subserosal fibroids grow on the outer surface of the uterus, intramural fibroids develop within the muscular wall, and submucosal fibroids protrude into the uterine cavity.
Different symptoms may occur depending on the fibroids' size, number, and location. Common signs consist of:
- Heavy menstrual bleeding
- Prolonged menstrual periods
- Pelvic pain or pressure
- Frequent urination
- Constipation
- Back pain
- Discomfort during sexual activity
No, many women with fibroids may not experience any symptoms and may not even be aware that they have fibroids unless detected during a routine medical exam or imaging test.
About two out of every three women will eventually experience uterine fibroids. While they can occur at any age, the 30- to 50-year-old age range is the most common for them to manifest.
Hormonal fluctuations, genetics, and environmental factors are among the many causes of fibroids. Hormonal imbalances, especially those involving the hormones progesterone and oestrogen, are likely to be a major contributing factor to their formation; however, the specific cause is unknown.
Multiple approaches are used to diagnose fibroids:
-
Pelvic exam: Your doctor will feel your abdominal and pelvic regions to look for abnormalities such as growths or enlargements of the uterus.
-
Blood tests: These can be performed to rule out other illnesses that might present with similar symptoms, like anaemia from heavy menstrual bleeding.
-
Imaging tests: Common imaging studies performed to identify fibroids include:
-
Ultrasound: This non-invasive technique can be used to determine the presence, size, and location of fibroids within the uterus by using sound waves to produce images of the uterus.
-
MRI (Magnetic Resonance Imaging): MRI provides detailed images of the uterus and fibroids, allowing for a more precise assessment of their size, number, and location. It is beneficial for evaluating larger or more complex fibroids and for planning treatment options.
-
CT (Computed Tomography) Scan: In certain circumstances, a CT scan may be performed to get cross-sectional images of the pelvis. These images can be useful in identifying and evaluating the characteristics of fibroids.
-
Treatment choices for fibroids consist of:
-
Medications: To help manage symptoms like pelvic pain and excessive bleeding, your doctor may prescribe medication. Nonsteroidal anti-inflammatory drugs (NSAIDs) or hormonal birth control (such as tablets, patches, or an IUD) can be used to help regulate your periods.
-
Minimally Invasive Procedures: Some minimally invasive procedures can help shrink or remove fibroids if your symptoms are more severe or if your medication isn't working well for you. These consist of:
-
Uterine Artery Embolisation (UAE): By preventing the fibroids' blood supply, this treatment gradually causes them to shrink.
-
MRI-guided Focused Ultrasound Surgery (MRgFUS): This minimally invasive technique heats and destroys fibroid tissue with high-intensity ultrasound waves.
-
Myomectomy: If you plan to have children in the future, this procedure can be an excellent option as it removes the fibroids while leaving your uterus in place.
-
Surgical Options: Your doctor may suggest a Hysterectomy in certain situations, particularly if the fibroids are very large or causing major symptoms. You will never be able to conceive again after this procedure, which eliminates the uterus and is a permanent treatment for fibroids.
-
Lifestyle Adjustments: Adopting good lifestyle practices, such as eating a well-balanced diet, getting regular exercise, and learning to manage your stress, can help you feel better overall and potentially lessen the symptoms of fibroid disease.
-
A Hysterectomy is a surgical operation in which the uterus is removed. Other reproductive organs like the cervix, ovaries, and fallopian tubes may also need to be removed during surgery, depending on the reason for the procedure. There are several forms of Hysterectomy:
-
Total Hysterectomy: This procedure involves the removal of the cervix and uterus.
-
Partial or Subtotal Hysterectomy: The cervix is left in place while only the top portion of the uterus is removed.
-
Radical Hysterectomy: The uterus, cervix, upper vagina, and its surrounding tissues are removed. When cancer is present, this is typically done.
-
Hysterectomy with Bilateral Salpingo-Oophorectomy: Both ovaries, both fallopian tubes, and the uterus are removed during a Hysterectomy with Bilateral Salpingo-Oophorectomy.
Several surgical techniques can be used to perform a Hysterectomy, including:
-
Abdominal Hysterectomy: A big incision is made in the lower abdomen to remove the uterus.
-
Vaginal Hysterectomy: Through the vagina, the uterus can be removed.
-
Laparoscopic Hysterectomy: A minimally invasive procedure where small incisions are made in the abdomen and a laparoscope (a thin, lighted tube) is used to guide the surgery.
-
Robotic-Assisted Laparoscopic Hysterectomy: A type of Laparoscopic Hysterectomy where the surgeon uses a robotic system to perform the procedure with enhanced precision.
A Hysterectomy is typically performed to treat conditions such as uterine fibroids, endometriosis, uterine prolapse, chronic pelvic pain, abnormal bleeding, and cancer of the uterus, cervix, or ovaries. It results in the permanent end of menstrual periods and the inability to become pregnant.
Yes, fibroids can impact fertility by obstructing the fallopian tubes or changing the uterus's structure. In many circumstances, treatment can aid in improving fertility.
No, surgery is not required in every case. Both minimally invasive surgeries and medicines are effective ways to manage many fibroids. Based on the patient's symptoms and reproductive objectives, an individualised treatment strategy is the best option.
Keeping up a healthy lifestyle that includes stress reduction, a balanced diet, and frequent exercise will help control symptoms. Avoiding high-oestrogen foods and managing weight can also be beneficial.
Yes, fibroids can recur after treatment, particularly if they are not completely removed. Regular follow-up and monitoring are essential to manage and address any new fibroid growth.
Home Mukundapur Specialities Obstetrics-and-gynaecology Fibroid-clinic

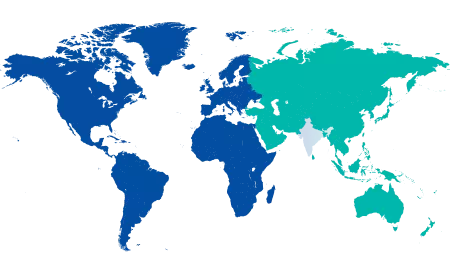
You’re on Our Indian Website
Visit the Global site for International patient services










