-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Surgical Treatment of Complex Anal Fistulas and Haemorrhoids
Surgical treatment of complex anal fistulas and Haemorrhoids in Mukundapur
An anal fistula is an infected anal gland that creates contact between the anus and the surrounding skin. It frequently starts as a perianal abscess, which is brought on by clogged glands that accumulate pus and bacteria. Pain, oedema, and discharge in the vicinity of the anus are the symptoms. Antibiotics and surgery are used in treatment to drain the abscess and mend the fistula. Serious consequences and repeated infections are possible outcomes of untreated fistulas. Timely medical attention is essential for effective treatment.
Haemorrhoids sometimes referred to as piles, are bulging and swollen veins in the rectum and anus. Most individuals may develop haemorrhoids, but until they get irritated, they usually don't create problems. Their size and discomfort can be attributed to various factors, such as straining during bowel motions, persistent constipation or diarrhoea, and extended periods of sitting. Itching, soreness, and a sensation of fullness or discomfort in the anal region are possible symptoms. Changing one's diet and lifestyle and using over-the-counter medications to relieve symptoms are common management strategies.
FAQ's
Anorectal disorders frequently result in fistulas, with a higher prevalence in men. About 75% of anal fistulas are caused by an infected gland that becomes an abscess and needs to be drained. As a result of this infection, an irregular tube linking the anus to the surrounding skin forms. For the fistula to be effectively managed, early detection and appropriate treatment are crucial.
Severe anal pain that is aggravated by bowel movements and other activities, as well as swelling, redness, and fluid discharge that may contain blood or pus, are indications of an anal fistula. Fever, pain with urination, and trouble managing bowel motions are less frequent symptoms.
The fistula's visibility differs when viewed in a mirror. Early medical evaluation is essential for a precise diagnosis and the right course of action to reduce discomfort and avoid consequences.
Fistulas can develop anywhere in the body, connecting organs or forming between an organ and the skin's surface. The formation of a fistula is frequently preceded by chronic inflammation or infection, which is often the result of prolonged tissue inflammation brought on by an injury or disease.
This persistent inflammation and infection can cause tissue erosion, which in turn facilitates the formation of a channel that allows drainage, typically pus, between the affected area and surrounding tissues. This abnormal passage can cause complications and require medical attention for proper management.
If left untreated, fistulas can become persistently infected, resulting in recurrent abscesses that cause excruciating pain. The fistula opening may momentarily close, but it frequently reopens due to a recurrent infection. Prolonged fistulas have the potential to grow longer and create intricate branching channels that are difficult to surgically treat.
Furthermore, although this consequence is uncommon, long-term fistulas are linked to a higher risk of anal cancer because of tissue erosion and persistent inflammation. Seeking prompt medical attention is essential to avoiding such long-term issues and ensuring successful anal fistula treatment.
Anal fistulas are categorised by medical professionals according to how close they are to the anal sphincter muscles, which are essential for bowel control. These types are supra sphincteric, which goes through the internal sphincter and around the external; extra sphincteric, which goes around both sphincters and often originates from the rectum; and superficial, which starts below the anal glands and avoids muscles.
Intersphincteric passes between the internal and external sphincters. Transsphincteric travels through both layers of sphincter muscles. Determining the best course of action for treating anal fistulas requires an understanding of these classifications.
Swollen veins in the rectum or around the anus are the cause of haemorrhoids, which can be external or internal. External haemorrhoids can cause pain, itching, and, on rare occasions, bleeding or clotting. Internal haemorrhoids originate in the rectum and usually do not hurt; however, they do usually cause bleeding.
When internal or external haemorrhoids extend outside the anus, it is known as a prolapsed haemorrhoid and can cause discomfort and bleeding. Getting medical help is crucial for effective symptom alleviation and management.
Anal fissures and haemorrhoids both have similar symptoms, such as pain, bleeding, and itching, but they have different underlying causes. Anal fissures are caused by tears in the anal lining, whereas haemorrhoids are caused by enlarged veins.
To discover the origin of your symptoms and ensure that you receive the right therapy, a healthcare practitioner may examine you physically and prescribe diagnostic testing. It needs a differential diagnosis to treat symptoms and manage them effectively.
Preventive steps can help reduce the chance of developing haemorrhoids. Refrain from sitting for extended periods or straining on the toilet, act quickly on bowel movements, and drink lots of water to stay hydrated. Frequent bowel movements can be encouraged by eating a diet rich in high-fibre foods such as fresh fruits, vegetables, and whole grains.
Gender-specific recommendations for fibre intake range from 25 grams for women to 35 grams for males each day. Bowel regularity is supported by regular physical activity. To prevent interfering with normal bowel function, laxatives and enemas should only be used under the supervision of a healthcare professional.
Home Mukundapur Specialities Organ-transplant Surgical-treatment-of-complex-anal-fistulas-and-haemorrhoids

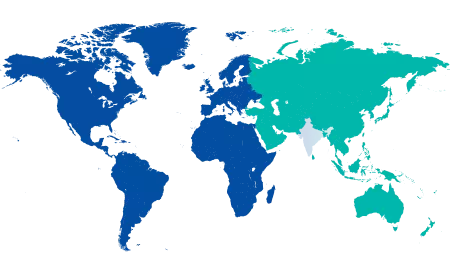
You’re on Our Indian Website
Visit the Global site for International patient services










