-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Paediatric Rheumatology
Best Rheumatology Hospital in Mukundapur
The diagnosis and treatment of autoimmune and inflammatory diseases affecting children's joints, muscles, and connective tissues are the main goals of paediatric rheumatology. These conditions are referred to as paediatric rheumatic diseases, including juvenile dermatomyositis, systemic lupus erythematosus (SLE), juvenile idiopathic arthritis (JIA), and systemic vasculitis. In paediatric rheumatology, the diagnosis entails a thorough assessment of systemic symptoms like fever or exhaustion as well as symptoms such as joint pain, stiffness, oedema, and rash. Diagnosis confirmation is aided by imaging scans, laboratory testing, and occasionally joint aspirations or biopsies. Treatment plans aim to maintain joint function, avoid complications, and ease symptoms. Usually, treatments such as corticosteroids, disease-modifying antirheumatic drugs (DMARDs), Biologic Therapy, and nonsteroidal anti-inflammatory drugs (NSAIDs) are used. Occupational and Physical Therapy is essential for preserving function and mobility. Continual multidisciplinary care involving paediatric rheumatologists, nurses, physical therapists, and social workers is essential to optimise treatment outcomes and promote the child's general development and well-being, as many rheumatic disorders are chronic.
FAQ's
The symptoms of juvenile idiopathic arthritis (JIA) may include tiredness, limited joint mobility, swelling, warmth, stiffness, and joint pain, especially in the morning. Some children might also exhibit rashes and fever, particularly in cases of systemic-onset JIA or eye inflammation like uveitis in oligo JIA. Growth spurts can result in growth issues in affected joints. The various subtypes of JIA have different symptoms, highlighting the importance of early detection and expert care to manage symptoms and prevent complications, such as joint damage.
Systemic lupus erythematosus (SLE) in children is diagnosed by assessing symptoms such as fever, rash, exhaustion, hair loss, renal involvement, cardiovascular involvement, respiratory involvement and joint pain in addition to vital tests including complement, ANA, and anti-dsDNA antibodies. Imaging could verify the participation of organs. According to the SLICC criteria, a diagnosis may only be confirmed if at least four clinical and immunological criteria are met. Few SLE patients can also have atypical presentations also, who do not fulfil the SLICC criteria. It's critical to rule out other conditions. Evaluation by a paediatric rheumatologist is essential for early diagnosis, efficient treatment, and the avoidance of long-term consequences.
Clinical characteristics and susceptibility to paediatric rheumatic disorders are influenced by genetics. Genetic predispositions are highlighted by family history, which helps with diagnosis. Treatment options may involve increased monitoring and take into consideration the family's response to the medications. Confirmation of diagnoses and prediction of illness severity are aided by genetic testing. In paediatric rheumatology, genetics and family history influence individualised care, hence enhancing treatment outcomes.
Juvenile dermatomyositis (JDM) treatment includes corticosteroids to reduce inflammation, immunosuppressants like methotrexate or mycophenolate mofetil for disease control, and biologics such as rituximab for resistant cases. Physical Therapy maintains muscle function, sun protection mitigates skin symptoms, and supportive care addresses nutritional and psychological needs. Early and tailored treatment optimises outcomes, though responses vary. Continuous monitoring and adjustment manage the disease effectively, aiming for remission and minimising medication side effects in paediatric patients.
Paediatric rheumatologists use clinical history, imaging (X-ray, ultrasound, MRI), lab testing (CBC, ESR, CRP, antibodies), physical examination, and joint fluid analysis to distinguish between different causes of paediatric joint pain. Diagnoses are made based on empirical therapeutic response: antibiotics for suspected infections or more rheumatologic testing for non-response. More testing (PCR, autoantibodies, etc.) helps provide a precise diagnosis. This methodical approach guarantees efficient care that is customised to the needs of every child.
Juvenile rheumatic disorders that go untreated can cause osteoporosis, growth impairment, joint deformity, organ damage, cardiovascular problems, psychosocial effects, infections, and an elevated risk of cancer. Preventive measures include aggressive early treatment with DMARDs and biologics, regular organ monitoring, psychosocial support, growth and bone health monitoring, cardiovascular risk factor management, vaccination, infection monitoring, and cancer screening. Involved children receive comprehensive care from paediatric rheumatologists, which guarantees early intervention and lowers long-term consequences.
Paediatric rheumatology collaborates closely with orthopaedics for joint evaluations and surgeries, immunology for managing biologic therapy and immunodeficiency screening, and dermatology for diagnosing and treating skin manifestations, as well as promoting photoprotection.
Comprehensive care is made easier by interdisciplinary clinics, and treatment and knowledge of paediatric rheumatic diseases are advanced by cooperative research and educational initiatives. These collaborations guarantee customised, integrated care to maximise results for kids with intricate rheumatoid diseases.
Children who suffer from long-term rheumatic illnesses must deal with difficulties including anxiety over the disease's course, mental distress, social isolation, problems with body image, educational failures, and strained family relationships. Regular counselling, educational interventions, encouragement for social integration, family counselling, transition planning, and clear disease information are some of the ways through which healthcare providers can support their patients' mental health. Children dealing with these complicated problems benefit from an all-encompassing approach that builds resilience, empowers families, and enhances their general quality of life.
Genetics, biologics, immunological mechanisms, biomarkers, digital health, psychological studies, and clinical trials are all contributing to the advancement of paediatric rheumatology research. Through the development of tailored treatments, improved illness monitoring, the integration of digital tools for remote care, and the application of holistic methods, these initiatives seek to improve quality of life. Researchers aim to improve treatment outcomes, lower complications, and improve the general well-being of children with rheumatic disorders by putting these advances into practice.
Home Mukundapur Specialities Paediatric-and-child-care Paediatric-rheumatology

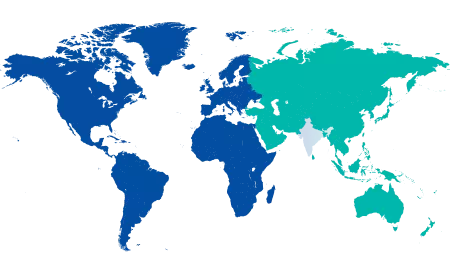
You’re on Our Indian Website
Visit the Global site for International patient services










