-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Hemodynamic Monitoring
Hemodynamic Monitoring in Mukundapur, Kolkata
Haemodynamic monitoring is essential for paediatric patients in critical condition who are frequently unstable as a result of cardiac failure, trauma, sepsis, or undergoing major surgery. This instability can result in organ failures, multiple organ failures, or even death. Therefore, haemodynamic monitoring is of utmost importance to prevent organ failure and enhance patient outcomes. Due to the diverse needs of paediatric patients in the ICU, a single mode of haemodynamic monitoring does not suffice. There are non-invasive modes like echocardiography and invasive modes like venous oximetry (SVO2). These monitoring modes employed for Hemodynamic Monitoring in Mukundapur, Kolkata, help detect inadequate tissue perfusion and oxygenation early before they become detrimental. They also prompt and guide resuscitation efforts.
FAQ's
Haemodynamic monitoring is essential when evaluating circulatory health and tissue perfusion in critically ill paediatric patients. In situations like shock, sepsis, and respiratory distress, it is crucial to assess fluid responsiveness, cardiac output, and vascular state. Haemodynamic monitoring is crucial in guiding therapeutic actions for complicated fluid balance management and postoperative care following heart procedures, ensuring adequate cardiac function and tissue perfusion. These uses highlight how important it is to enhance clinical results and customise treatment plans for sick children.
To prepare for haemodynamic monitoring, it's important to explain the procedure to the child with age-appropriate language. Refrain from allowing the child to eat or drink anything, including gum and candy, for at least four hours before the test, and give medications only with a small sip of water if necessary. Never discontinue medications without consulting your child’s healthcare provider first. These steps ensure optimal conditions for accurate haemodynamic monitoring.
Throughout the examination of haemodynamic monitoring:
-
On an examination table, your child will be made to lie on their back.
-
An IV will be given to your child to administer a radioactive isotope.
-
The tracer will be injected into the IV by your physician before each round of pictures. During the test, additional drugs could be administered to the child via an IV.
-
The gamma camera will be placed across the child’s chest by your healthcare professional. It will capture pictures while the child remains still. The procedure takes about three hours to complete.
One of the invasive techniques of haemodynamic monitoring is the Pulmonary Artery Catheter (PAC):
-
A catheter is inserted via the jugular, subclavian, or femoral vein, extending to the pulmonary artery, which directly measures pressures: CVP, PAP, and PAOP (or wedge pressure) and is used for blood sampling for SvO2 and also for continuous monitoring via fibre optic reflectometry.
-
CO is measured by thermodilution with cold saline boluses or heating coils.
-
Provides calculated variables: systemic and pulmonary vascular resistance, and ventricular stroke work.
-
Intracardiac electrodes for monitoring electric activity and assessing RVEF and CEDV.
-
Challenges include CO averaging, inter-observer variability, and misinterpretation of tracings.
-
Valuable in right ventricular heart failure or pulmonary hypertension for direct pressure measurement.
Less-invasive techniques include Transpulmonary Thermodilution (Utilises central venous catheter and arterial line for CO measurement.
-
Intermittent CO measured via transpulmonary thermodilution; continuous CO from arterial pulse contour analysis.
-
Provides real-time assessment of stroke volume and CO variations, Transpulmonary Dye Dilution, Ultrasound Flow Dilution, and Pulse Contour Analysis.
-
Techniques vary in calibration methods, measurement capabilities, and limitations.
-
Pulse contour analysis methods estimate CO from pulse pressure; limitations exist in unstable patients or under vasoactive drug influence.
-
Respiratory-derived cardiac output monitoring measures CO using the CO2 rebreathing method, limited to sedated patients with controlled ventilation.
-
Transesophageal echocardiography offers operator-dependent assessment but lacks continuous monitoring capability.
Arterial Blood Pressure
-
Blood pressure is a common measure of haemodynamic instability, both high and low.
-
The blood pressure readings must be correlated with the clinical symptoms.
-
Does not allow continuous monitoring.
Transthoracic Echocardiography (TTE):
-
It is an operator-dependent technique.
-
CO was measured using pulsed-wave Doppler velocity in the left ventricular outflow tract (LVOT).
-
Measurements at other locations like the mitral valve annulus, ascending aorta, RVOT, and pulmonary artery are less validated.
-
Accuracy may be affected by pulmonary arterial hypertension.
Non-invasive Pulse Contour Systems:
-
Includes the bioimpedance method.
-
Utilises skin electrodes to apply a small electrical current.
-
Changes in the impedance or volume of conducting tissues are measured.
-
The impact of intrathoracic blood volume on impedance provides CO estimation.
The use of invasive techniques for haemodynamic monitoring, which is essential in critical care, poses hazards including bleeding, infection, and arrhythmias. Non-invasive methods might be uncomfortable or difficult to use accurately. Overarching issues include allergic responses, equipment failures, and psychological effects. Strict aseptic procedures, watchful observation, and quick action are all part of prevention. Frequent training guarantees staff proficiency, encourages safe procedures, and improves patient outcomes when the patient is under haemodynamic surveillance.
Home Mukundapur Specialities Paediatric-intensive-care-unit Hemodynamic-monitoring

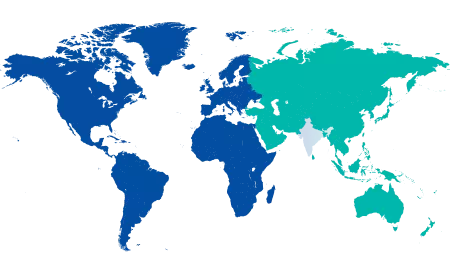
You’re on Our Indian Website
Visit the Global site for International patient services










