-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Tracheostomy Care and Home Ventilation
Tracheostomy Care and Home Ventilation
The procedure done to provide an alternate air passage in the trachea for patients with blocked or reduced breathing is called a Tracheostomy. Tracheostomy care is very important because it involves the maintenance and management of a surgical opening in the windpipe (trachea). This involves the following things:
-
The tracheostomy site should satisfy hygienic conditions involving its functioning and comfort.
-
Cleaning the area around the tracheostomy tube, changing dressings, and suctioning the secretions.
-
Careful watching for indications of infection and ensuring the correct positioning of the patient's head and neck are also included.
Home Ventilation: The provision of respiratory support and therapy for individuals with breathing difficulties at home is called home ventilation. Tracheostomy care and home ventilation in Mukundapur include specific medical equipment such as ventilators, which can be non-invasive (like masks and nasal prongs) or invasive (like tracheostomy tubes). This is beneficial for paediatric patients, as it enhances their comfort level.
FAQ's
A Tracheostomy can cause a variety of immediate, early, and late problems, despite being a life-saving procedure. Bleeding, pneumothorax, subcutaneous emphysema, and tracheal damage are examples of immediate issues. The early consequences include the development of granulomas, displacement of the tube, infection, and obstruction. Speech and swallowing difficulty, scarring, tracheocutaneous fistula, tracheomalacia, tracheoesophageal fistula, chronic infection, and tracheal stenosis are examples of late complications. Other significant factors to take into account include care dependence and psychological effects. Careful observation and professional medical attention are essential to lowering these risks and guaranteeing the best possible patient results.
-
Obturator Tightness: The trach tube may need to be replaced if the obturator, which is the instrument used to guide the tube during insertion, seems too tight or difficult to implant.
-
Misalignment of the Trach Shaft: This indicates that the tube may not be fitting well or may have moved, requiring a new tube, if the trach shaft is not centred within the stoma.
-
Discolouration: The material's integrity and cleanliness may be jeopardised if there is a discernible change in the trach tube's colour, such as yellowing or darkening.
-
Faded Markings: The trach tube's markings, which aid in determining its dimensions and location, have to be distinct and readable. It is challenging to guarantee accurate placement with faded marks, which might indicate the need for another tube.
-
Trach ties are crucial for securing the trach tube in place and should be kept clean and dry to prevent skin irritation, sores, and infections around the neck area.
-
Trach ties, which are usually composed of twill cotton or fabric and fastened with a velcro clasp, are essential to preserving the stability of the trach tube.
-
It's crucial to keep the trach tube from unintentionally coming loose when replacing the ties. It is best to have two individuals do this procedure: one to clean the skin and reattach the ties, and the other to keep the trach in place.
-
In order to avoid inadvertently dislodging the trach tube, knot the clean ties before removing the old ones if help is not available. This safety measure guarantees that the tube stays firmly in place during the replacement process.
First, empty the cuff of all air or distilled water. After that, re-inflate the cuff using the recommended pressure or pure water. Hold off for a short while. If there is a leak, then:
1. Empty the cuff of all air or distilled water again.
2. If the amount taken out was less than expected, re-inflate with the appropriate amount.
3. You can attempt this if your cuff is full of air. While the pilot balloon is "inflated," place it in a cup of water. There is a leak in the pilot line or pilot balloon if bubbles are visible.
4. If there is still a leak, the trach tube needs to be replaced.
You might not be able to breathe deeply enough on your own, so a ventilator could be necessary to help flow air into and out of your lungs. The ventilator can assist with your breathing entirely (total assistance) or only in part.
Own respiration (with some assistance): PEEP pressure, which is an additional pressure that most ventilators can provide, keeps the lungs open and prevents the collapse of the air sacs. A ventilator and mouthpiece, a ventilator and mask, or a ventilator and trach tube can all be used for mechanical ventilation.
Even though mechanical ventilation might save lives, several issues can arise and impact different organ systems. Common difficulties include delirium, infections, muscular weakness, gastrointestinal bleeding, acute renal damage, hypotension, reduced cardiac output, infections, and respiratory complications such as barotrauma and ventilator-associated pneumonia. Concerns can include psychological effects including PTSD and anxiety, aspiration, oxygen toxicity, and difficulty weaning. To reduce these hazards and enhance patient outcomes, diligent treatment and routine monitoring are crucial.
During a home ventilator failure, prompt action is essential. Assess the patient’s condition and airway, switch to manual ventilation if necessary, and contact emergency services or healthcare providers immediately. Ensure the ventilator is powered and check for malfunctions. Monitor vital signs closely, maintain oxygen supply, and prepare for potential hospital transport. Following a pre-established emergency plan, documenting actions taken, and reviewing incidents afterwards are critical for patient safety and effective management of ventilator failures at home.
For patients experiencing respiratory failure, mechanical ventilation either supplements or substitutes for spontaneous breathing. Volume-Controlled Ventilation (VCV), Pressure-Controlled Ventilation (PCV), Assist-Control Ventilation (ACV), Pressure Support Ventilation (PSV), High-Frequency Oscillatory Ventilation (HFOV), Pressure-Regulated Volume Control (PRVC), Continuous Positive Airway Pressure (CPAP), and Bi-Level Positive Airway Pressure (BiPAP) are some of the important modes. Every approach meets certain clinical requirements, has benefits and drawbacks, and necessitates customised patient care and observation.
Home Mukundapur Specialities Paediatric-intensive-care-unit Tracheostomy-care-and-home-ventilation

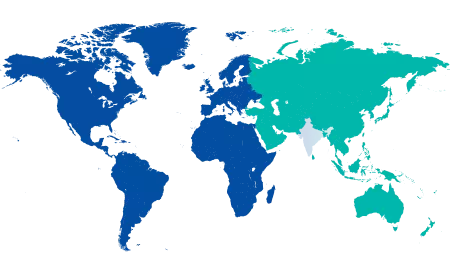
You’re on Our Indian Website
Visit the Global site for International patient services










