-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Dialysis Access
Dialysis Access Surgery in Mukundapur
For patients receiving Hemodialysis, dialysis access is essential since it offers a means of purifying blood outside of the body. Arteriovenous (AV) fistulas, AV grafts, and central venous catheters (CVCs) are the three main approaches to gaining dialysis access.
-
AV fistulas include surgically joining an artery and a vein, usually in the arm. They are preferred due to their durability and lower risk of problems.
-
When AV fistulas are not feasible, synthetic material AV grafts serve as a backup plan. They serve to join an artery and a vein, but they are more vulnerable to clotting and infection.
-
If urgent dialysis is required or other AV alternatives are not accessible, CVCs—which are temporary solutions—are put into major veins in the neck, chest, or groyne. They do, however, have a higher chance of infection.
Vein size, treatment length, and vascular health are among the criteria that influence selection. For successful treatment, to minimise problems, and to improve patient well-being throughout their hemodialysis journey, it is imperative to ensure appropriate dialysis access.
FAQ's
Arteriovenous (AV) fistulas are the preferred option for long-term dialysis access because of their affordability, durability, reduced risk of infection, and enhanced blood flow. Compared to other alternatives, AV fistulas have a longer lifetime, which lowers problems and medical expenses. Through the process of vein growth and strengthening, AV fistulas improve patient outcomes and quality of life by offering dependable access to effective Hemodialysis treatments.
The choice between arteriovenous fistulas (AVFs) and arteriovenous grafts (AVGs) for dialysis access is impacted by several variables, including the patient's vascular anatomy, vascular health, prior access history, comorbidities, anticipated dialysis duration, and preference. Due to their longevity, AVFs are recommended for long-term dialysis; however, AVGs can be used for short- to medium-term access or in situations where creating an AVF is not practical. Access selection is guided by patient-specific traits and preferences, hence improving results.
Central venous catheters (CVCs) are flexible, minimally invasive, and provide instant vascular access for Hemodialysis. However, in comparison to permanent access alternatives such as AVFs and AVGs, they have a higher risk of infection, thrombosis, and morbidity. Their usage is further limited to temporary or transitional access options due to their short-term reliability and risk of central venous stenosis. All things considered, CVCs are essential transient access devices in Hemodialysis, but they must be closely watched for potential hazards.
An artery and a vein in the arm are surgically connected to create an arteriovenous fistula (AVF), usually in the wrist or elbow area. By rerouting arterial blood flow into the vein, this connection makes the vein larger and more appropriate for hemodialysis access. The AVF can be used for dialysis therapy once it has matured. Blood is extracted and returned through the AVF during hemodialysis sessions, allowing for the effective removal of waste materials and extra fluid from the circulation.
What are the potential complications associated with arteriovenous grafts, and how are they managed?
Complications from arteriovenous grafts (AVGs) used for dialysis access include thrombosis, infection, stenosis, the creation of pseudoaneurysms, and graft migration. Thrombectomy, Antibiotics medications, Angioplasty, Pseudoaneurysm Repair, or Graft Revision are among the treatment options that help overcome these complications. Maintaining good dialysis results and preventing complications need routine observation.
Central venous catheters (CVCs) are essential for emergency dialysis access, as a bridge to permanent access, or for interim access as AVF/AVG mature. While placing a CVC, factors to be taken into account are vein selection, infection control, catheter size and type selection, problem avoidance, and close patient observation. CVCs are useful for quick access, but they also require careful management to reduce problems and maximise results.
Maintaining and monitoring dialysis access sites regularly is essential to avoiding problems and improving patient outcomes. This entails regular evaluations conducted during dialysis sessions, clinical follow-ups every one to three months, recurring ultrasonography surveillance to evaluate patency and identify problems, tracking access flow rates, taking part in surveillance initiatives, educating patients on self-monitoring, and acting promptly in the event of abnormalities. These steps improve patient safety and well-being and guarantee efficient access management.
Reduced thrill or bruit feeling, oedema, soreness, skin discolouration, and difficulty with dialysis are indicators of dialysis access malfunction. To ensure good access function and dialysis results, prompt medical treatment is required to address possible problems such as infection, thrombosis, or stenosis. Maintaining access lifespan and preventing new problems need early detection and treatment.
Home Mukundapur Specialities Radiology Dialysis-access

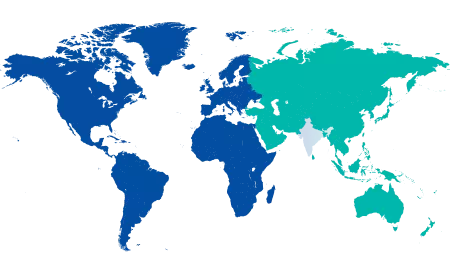
You’re on Our Indian Website
Visit the Global site for International patient services










