-
Centre of
Excellence
Centre of Excellence
- Accident and Emergency Care
- Cancer Care/Oncology
- Cardiology
- Cardiothoracic Vascular Surgery
- Gastrointestinal Science
- Laparoscopic Surgery
- Liver Transplantation Surgery
- Nephrology
- Neurology
- Neurosurgery
- Obstetrics and Gynaecology
- Organ Transplant
- Orthopaedics
- Paediatric And Child Care
- Rheumatology
- Spine Care
- Urology
Other Specialities
- Allergy and Immunology
- Andrology
- Anesthesiology
- Bone Marrow Transplantation
- Children’s Airway & Swallowing Centre
- Clinical Psychology
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Ear Nose Throat
- Electrophysiology
- Fetal Medicine
- General Medicine
- General Surgery
- Genetics
- Geriatric Medicine
- GI Surgery
- Gynaec Oncology
- Hemato Oncology
- Hematology
- Hepatobiliary Surgery
- ICU and Critical Care
- Infectious Disease
- Internal Medicine
- Interventional Radiology
- Kidney Transplant
- Laboratory Medicine
- Lactation
- Medical Gastro
- Medical Oncology
- Microbiology
- Minimal Access Surgery
- Neonatology & NICU
- Nutrition And Dietetics
- Ophthalmology
- Oral Maxillo Facial Surgery
- Paediatric Cancer Care
- Paediatric Cardiology
- Paediatric Endocrinology
- Paediatric General Surgery
- Paediatric Intensive Care Unit
- Paediatric Neurology
- Paediatric Surgery
- Paediatric Urology
- Pain Medicine
- Parkinson Disease and Movement Disorder
- Pathology
- Pediatric Bone Marrow Transplant
- Pharmacy
- Physiotherapy
- Plastic And Cosmetic Surgery
- Podiatric Surgery
- Psychiatry
- Psychology
- Pulmonology (Respiratory and Sleep Medicine)
- Radiology
- Rehabilitation Medicine
- Renal Sciences
- Reproductive Medicine
- Robotic Assisted Surgery
- Surgical Gastro
- Surgical Oncology
- Transfusion Medicine
- Vascular and Endovascular Surgery
- Doctors
- Mukundapur
- International Patients



Clinics








- Self Registration
- Mars - Ambulance
- Corporate & PSU
- Insurance Helpdesk
- Awards And Achievements
- Careers
- Contact Us

Renal Replacement Therapy
Renal Replacement Therapy in Mukundapur
Renal Replacement Therapy (RRT) is a type of treatment that substitutes the kidneys' natural ability to filter blood. It is used to treat acute renal injury and chronic kidney disease, together with other conditions known as kidney failure. Hemofiltration, hemodiafiltration, and dialysis (hemodialysis or peritoneal dialysis) are three different methods of filtration of blood that can be done with or without equipment as part of Renal Replacement treatment. Kidney Transplantation, the most advanced type of replacement in which a donor kidney replaces the damaged kidney, is also part of Renal Replacement Therapy. In individuals with renal failure, nonendocrine kidney function is replaced by Renal Replacement Therapy. All of these treatment modalities use filtration through permeable membranes and dialysis to exchange solutes and remove fluid from the blood.
Chronic kidney disease is often considered life-extending, with early management and successful transplantation of a compatible graft leading to favourable clinical outcomes. In acute kidney injury cases, individuals can survive for years with good kidney function, provided they respond well to dialysis, receive a transplant quickly, and have no other significant health issues. At Manipal Hospitals, Mukundapur, we have a team of experienced nephrologists who employ advanced treatment methodologies to provide enhanced treatment outcomes.
FAQ's
Patients can take control of their health in the early stages of chronic kidney disease by following a healthy diet and taking their prescription drugs as directed. It may be necessary to combine these treatments with other therapies if kidney function drops to less than 15% of normal. In such cases, Renal Replacement Therapy is needed to maintain the health of the kidneys. The different types of Renal Replacement Therapy are:
1. Hemodialysis
2. Peritoneal Dialysis
3. Continuous Renal Replacement Therapy (CRRT)
4. Kidney Transplantation
Dialysis is a medical intervention used to treat renal disease. Regretfully, it cannot completely restore normal kidney function or treat kidney disease. It is a process that artificially eliminates waste and extra water from the blood. The body benefits from this procedure by operating normally. Hemodialysis and peritoneal dialysis are the two forms of dialysis.
Dialysis is used in two situations:
-
Acute kidney injury (AKI): Acute kidney damage is described as a brief, quick episode of renal failure or damage. Intravenous (by the vein) fluids are typically used in a hospital environment to treat acute kidney injury (AKI). Dialysis might also be required in extreme situations for a brief period of time until the kidneys recover.
Renal failure is defined as having an estimated glomerular filtration rate (eGFR) of less than 15 mL/min and the remaining 10-15% of kidney function. Your kidneys can no longer sustain you on their own at this point and need outside assistance to stay alive. End-stage kidney disease (ESKD) is another term for this. Dialysis cannot treat renal illness; it can only partially replace the functions of functioning kidneys in cases of kidney failure. If you have end-stage kidney disease (ESKD), you will only require dialysis until you are able to receive a Kidney Transplant.
Some of the functions that your kidneys normally carry out to maintain the balance of your body are fulfilled by dialysis, including:
-
Eliminating excess fluid and waste from your body to stop it from building up
-
Maintaining healthy blood mineral levels, including calcium, salt, potassium, and bicarbonate
-
Assisting in blood pressure regulation
Hemodialysis involves the removal of waste and excess fluid from your blood using a dialyser (filtering equipment) and the subsequent injection of the filtered blood back into your body. A small operation is required to make a vascular access site—a hole into one of your blood vessels—usually in your arm before you can begin hemodialysis. It's crucial to have this access point so that blood may be easily removed from your body, passed through the dialyser, and then returned to it. Dialysis can be performed at home or in a facility. This treatment may require four hours to complete and may be needed for three days a week. Depending on their unique requirements, some patients could require longer therapy.
Instead of using dialyser equipment, your blood is filtered internally during peritoneal dialysis. The peritoneum, which is the lining of your abdomen, serves as a filter for this type of dialysis. A small amount of surgery is required to implant a catheter (soft tube) in your abdomen prior to beginning peritoneal dialysis. Dialysate, a cleansing solution consisting of a blend of water, salt, and additional ingredients, is progressively injected into the abdomen via the catheter during every session. The dialysate acts almost like a magnet, drawing additional fluid and waste items from the blood vessels and into the abdominal area when your blood flows naturally through the area.
The length of your dialysis stay varies based on your underlying medical conditions, your adherence to your treatment plan, and a number of other factors. Patients on dialysis typically have a 5–10 year life expectancy.
Providing comfort care while allowing the disease to progress naturally is known as non-dialytic care. Rather than undergoing dialysis, people manage their symptoms with the help of medical specialists and by adhering to a prescribed diet and drug schedule. Non-dialytic care is opted for by individuals in the following cases:
-
The end of life is drawing near for patients with end-stage renal disease and they may find that their life expectancy is shortened, whether they are receiving dialysis or not.
-
Patients may believe that Renal Replacement treatment is not the best course of action for them during this period, as it is not necessary that it can improve their quality of life.
However, patients are free to discontinue or not begin Renal Replacement treatment in certain circumstances. Patients must be well informed about all available alternative therapies and the effects of each type.
Individuals must talk to their doctor about their sentiments and concerns before deciding on conservative treatment. Your physician will discuss conservative care with you and how it impacts your health.
A Kidney Transplant is a surgical procedure to replace an improperly working kidney with a healthy one. The person who donates a healthy kidney is known as a donor. The kidney can be donated by a person who is alive (a living donor), such as a friend, spouse, or relative, or it can come from a dead person (a deceased donor), who may not be someone you know.
The diseased kidneys remain inside your body, while the healthy kidneys are transferred to the front side of the body, into the lower abdomen. The transplanted kidney then does the work of filtering the waste from your body.
One may need a Kidney Transplant if they are suffering from end-stage renal disease (ESRD), which is also known as kidney failure. It sometimes becomes necessary to get relief from the following symptoms of ESRD through a Kidney Transplant, such as:
- Urinary infections
- Kidney failure, caused by diabetes or high blood pressure
- Presence of cysts in the kidney (polycystic kidney disease)
- Infection of the kidney's filtering unit, the nephron (glomerulonephritis)
- Diseases of the immune system
- Inherited diseases of the kidney
Home Mukundapur Specialities Renal-sciences Renal-replacement-therapy

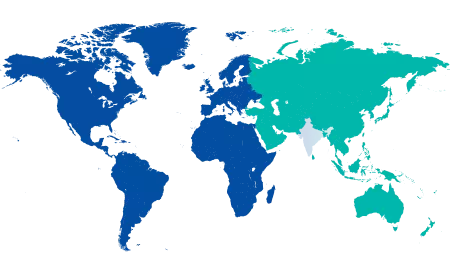
You’re on Our Indian Website
Visit the Global site for International patient services










